Most women with cervical cancer in Kenya present in stages three and four, when treatment is difficult, expensive, and sometimes unavailable, while the HPV vaccine offers lasting protection.
The government has urged parents to allow their daughters to receive the Human Papillomavirus (HPV) vaccine, citing its critical role in preventing cervical cancer, the second most common cancer among Kenyan women.
Speaking during the launch of the National Cervical Cancer Elimination Plan (2026–2030) in Nairobi on January 15, 2026, Health Cabinet Secretary Aden Duale described cervical cancer as a “silent epidemic” that continues to devastate families despite the availability of effective prevention tools.
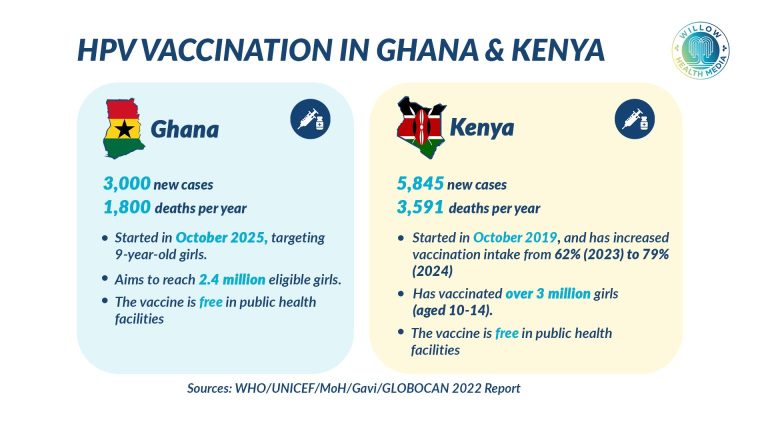
“Each year, nearly 6,000 new cases are diagnosed and over 3,500 Kenyan women die from cervical cancer,” Duale said. “Because this disease is almost entirely preventable, its persistence is a stark marker of health inequity that we are determined to end.”
The new plan introduces major policy changes, including Kenya’s transition from a two-dose to a single-dose HPV vaccination schedule, implemented in November 2025 following World Health Organization (WHO) recommendations. The move is aimed at vaccinating 90 per cent of girls against HPV by age 15.
“This evidence-based shift allows us to reach more girls, reduce missed opportunities, and accelerate our progress,” Duale said.
The 2026-2030 Cervical Cancer Elimination plan aligns Kenya with WHO’s 90-70-90 targets
The HPV vaccine is now offered free of charge to girls aged 10-14 years at public health facilities nationwide. Duale urged parents and caregivers to trust the vaccine, saying it is “safe, effective, and rigorously tested.”
“It has protected millions of women worldwide. Elimination begins with prevention, and we must ensure that no eligible girl is left behind,” he said.
The launch, held to mark National Cervical Cancer Awareness Month, brought together policymakers, health professionals, county officials, civil society groups, development partners, and cancer survivors.
The 2026-2030 plan aligns Kenya with WHO’s 90-70-90 targets, which seek to vaccinate 90 per cent of girls against HPV by age 15; screen 70 per cent of women using high-performance tests and ensure 90 per cent of diagnosed women receive timely and effective treatment.
“Our roadmap is anchored in a proven, three-fold strategy: primary prevention through vaccination, secondary prevention through timely screening, and a firm commitment to ensuring every diagnosed woman completes her treatment,” Duale said. “This continuum of care is our blueprint.”
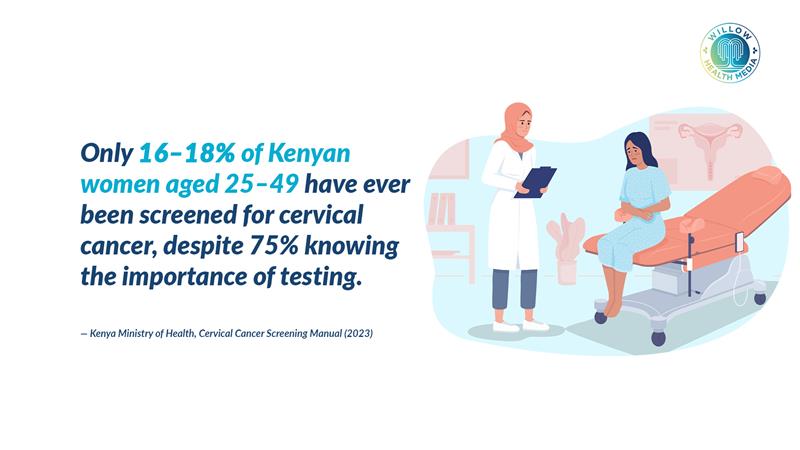
While prevention through vaccination is central, early detection remains a major challenge. Cervical cancer screening rates among women aged 25-49 have improved from 11 per cent in 2018 to 42 per cent in 2024 according to the Ministry of Health, which is still well below the 70 per cent target.
To close the gap, the plan prioritizes strengthening primary healthcare services across all 47 counties, expanding HPV DNA testing, and introducing self-sampling techniques. Digital health platforms will also be used to track screened patients and improve follow-up.
“We commit to ensuring that every woman is screened by age 35, and again by age 45, regardless of her location or economic status,” Duale said.
A key pillar of the plan focuses on ensuring timely treatment for women diagnosed with cervical disease. According to Dr Alfred Mokomba, a consultant gynaecologist oncologist, most patients present too late.
Equipment breakdowns and shortages of skilled personnel continue to limit access for women
“Most women present in stages three and four, when treatment is difficult, expensive, and sometimes unavailable,” he said, noting that cultural stigma around abnormal vaginal bleeding discourages early care-seeking.
He added that systemic delays worsen outcomes. “By the time a woman is seen at a level one or level two facility, it can take months for diagnosis and referral.”
Radiotherapy, which is the mainstay treatment for advanced cases, is currently available at Kenyatta National Hospital, Kenyatta University Hospital, Nairobi Hospital, MP Shah Hospital, and county referral hospitals in Nakuru, Mombasa, and Garissa. However, equipment breakdowns and shortages of skilled personnel continue to limit access, particularly for women in rural areas.
“Screening helps us identify cases early so they can be treated successfully. Vaccination prevents the disease from occurring in the first place. Together, they are our most powerful tools against cervical cancer,” Dr Mokomba said.
The national elimination plan is supported by health financing reforms under the Social Health Authority (SHA), which allow direct reimbursement to health facilities, helping sustain screening and treatment services while easing the financial burden on families.
“Cancer treatment should not push families into poverty,” Duale said. “Through these reforms, we aim to make timely, affordable, and uninterrupted care a reality.”
Duale called for cross-sector collaboration, urging the Ministry of Education to integrate HPV vaccination into school health programs, and for county governments to ensure commodities and motivated health workers are available.
Kenya records about 5,845 new cervical cancer cases and up to 3,600 deaths annually
Civil society groups, including the Kenya Network of Cancer Organizations (KENCO), and cancer survivors were also recognised for their role in building trust and combating stigma.
According to the Global Cancer Observatory (GLOBOCAN) 2022, Kenya records about 5,845 new cervical cancer cases and up to 3,600 deaths annually. Data from the Kenya Medical Research Institute (KEMRI) Cancer Registry shows women aged 45-59 account for 43 per cent of cases, followed by those aged 30-44 at 35 per cent; suggesting HPV infection often occurs much earlier in life.
“Despite being highly preventable, cervical cancer continues to claim the lives of productive women, often leaving families fractured and communities diminished,” Dr Mokomba said, urging greater investment in radiotherapy services outside Nairobi.
The National Cervical Cancer Elimination Plan (2026-2030) is Kenya’s first costed, results-driven roadmap to address prevention, early detection, treatment, and long-term follow-up.
“Let us be the generation that ends cervical cancer in Kenya,” Duale said. “Let us leave no girl unvaccinated, no woman unscreened, and no patient untreated. Together, we can, and we will, eliminate cervical cancer from our country.”