“All patients with NHIF bills before October 1, 2024, will have their bills paid by NHIF”
-Dr Abdi Mohammed, SHA chair
By Nancy Nzau
As Kenya enters the second week of the new health financing system, the Social Health Authority (SHA) has assured Kenyans it will continue closing all the emerging gaps during its implementation.
The Social Health Act is intended to provide comprehensive health coverage, but it has attracted significant debate, uncertainty, and controversy since inception, especially concerning its effect on existing healthcare structures, stalled registration systems and tariff packages.
Many patients who visited hospitals since October 1, when the Social Health Insurance Fund (SHIF) officially replaced the National Hospital Insurance Fund (NHIF) said they could not register or access services as the system was experiencing persistent downtimes.
The hospital administrators were also in the dark and had to turn away patients who couldn’t afford to pay out-of-pocket for health services. “We can’t access the patients’ details on our system, and even when we manage to register patients to SHIF, we cannot proceed. So far, we’re doing absolutely nothing,” lamented an administrator at Mbagathi Hospital in Nairobi. “We’re in a blackout. Patients are going home unattended, or they go to the cashier.”
Paul Ng’ang’a, who had brought his wife, Mary Ng’ang’a, for a dialysis session at Mbagathi Hospital said “we are ready to shift to SHIF, but when we try to register, it says the service is currently unavailable.
Addressing the issue of registration at a press briefing this Sunday, SHA chairperson Dr Abdi Mohamed said “during the initial days of the rollout, we experienced challenges on the e-claim portal, particularly on member verification and claim processing” but Kenyans can now register in droves as the portal is up and running after they resolving system challenges and successfully onboarding all public hospitals and many private and faith-based facilities.

Dr Mohamed confirmed that as of October 6, 2024, SHA had “registered a total of 12,704,548 members. This number includes verified members who are under the defunct NHIF and who have been transitioned to the Social Health Authority as per legal notice” he said and noted that most beneficiaries were not adding their dependents to access healthcare.
Dr Mohammed said that public hospitals from Levels 2 to 6 have been contracted and are already offering services to SHA-registered beneficiaries including 1,442 private and faith-based health facilities that have been contracted and are already offering services. ”All registered SHA beneficiaries and their dependents are entitled to free access to primary healthcare services under the primary health care fund at Level 2 dispensaries, 3 health centres and select Level 4 health facilities and emergency services in all health facilities.”
Dr Abdi said the list of all health facilities contracted and offering services is available on the SHA website, further urging the private and faith-based facilities to return duly signed contracts by Tuesday, October 8, 2024.
He urged patients who spent money on treatment on October 1, to contact the authority for reimbursement and “all patients whose admissions or procedures commenced after September 30, 2024, will have their bills settled under SHA. There is no lacuna,” he said adding that
“All patients where NHIF had given an undertaking before 1st October will have their bills paid by NHIF.”
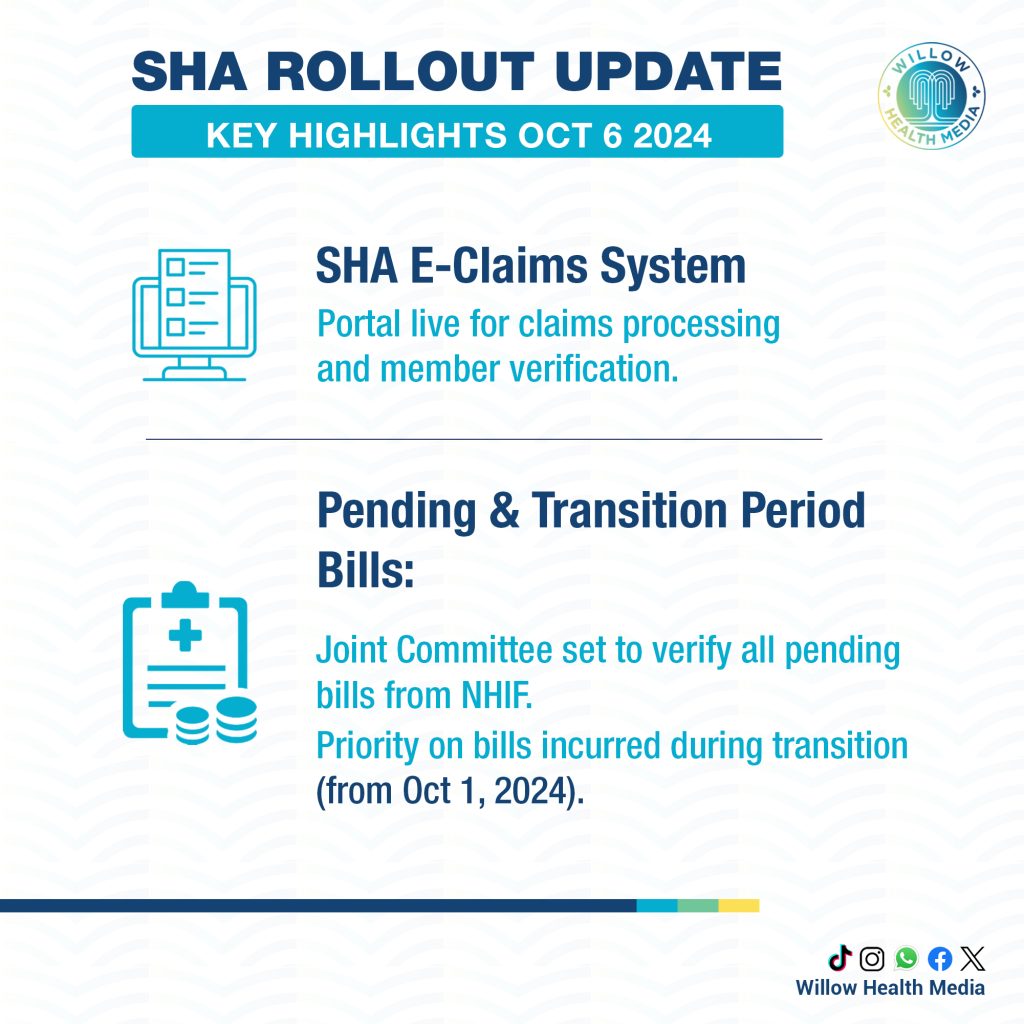
Dr Brian Lishenga, the Rural Private Hospitals Association of Kenya (RUPHA) chair, expressed confidence in SHA’s efforts to iron out the e-claim system and members “should be able to claim through the SHA portal within the next 24 hours” and any other claims incurred since the transition began “will be prioritised and claims honoured.”
Chair of the Kenyan Healthcare Federation, Dr. Kanyenje Gakombe, said that despite the transition challenges, he was happy with some changes, especially the 5% administrative costs assigned for SHA staff leaving the remaining chunk (95%) to cater to the patients’ needs.
“NHIF used to spend 80% of the money on itself, 10% on fraud and 10% on us. This is public information,” he said. He commended SHA for setting up transparency structures such as a tariff board to review medical service costs and an appeal tribunal for individuals and providers as “In the past, NHIF has been judge, jury and executioner.”
He also lauded the provision of open feedback channels, appealing to Kenyans to use the government scorecard to give feedback on whether they are getting quality care or not, even as representatives from various associations promised to hold SHA accountable.





















