Have you ever heard of haemophilia?
It is rare. It is serious. And it’s a genetic condition that interferes with the blood’s natural ability to clot.
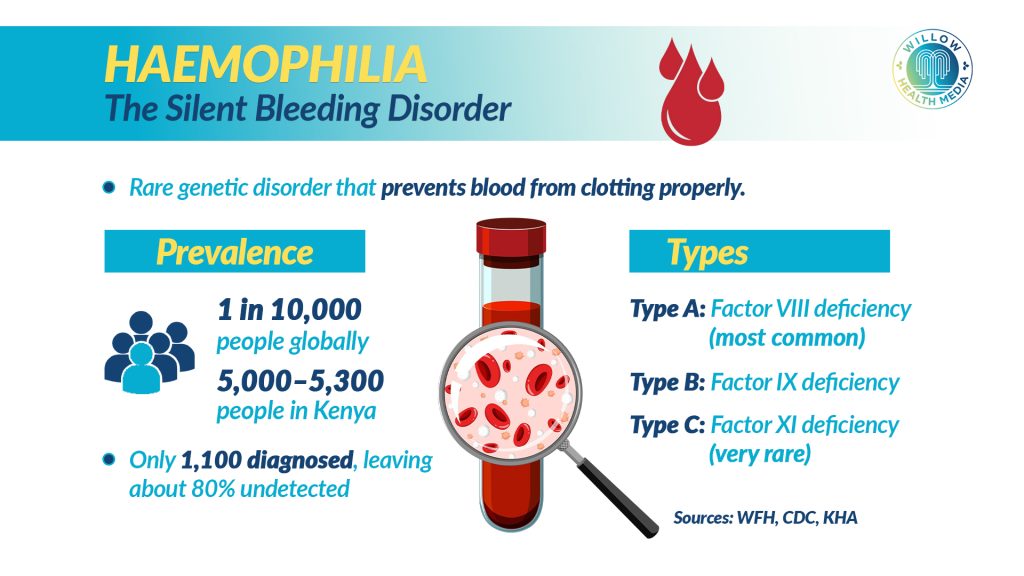
Globally, haemophilia affects about 1 in every 10,000 people. In Kenya, many live with it unknowingly.
According to Dr Kibet Peter Shikuku, the country has roughly 1,100 diagnosed haemophiliacs out of an estimated 5,000 patients – meaning nearly 80% remain undetected.
Here is how it works: when you get a cut, platelets rush to the site to form a plug. But without clotting factors – particularly factor 8 or 9, the bleeding simply doesn’t stop.
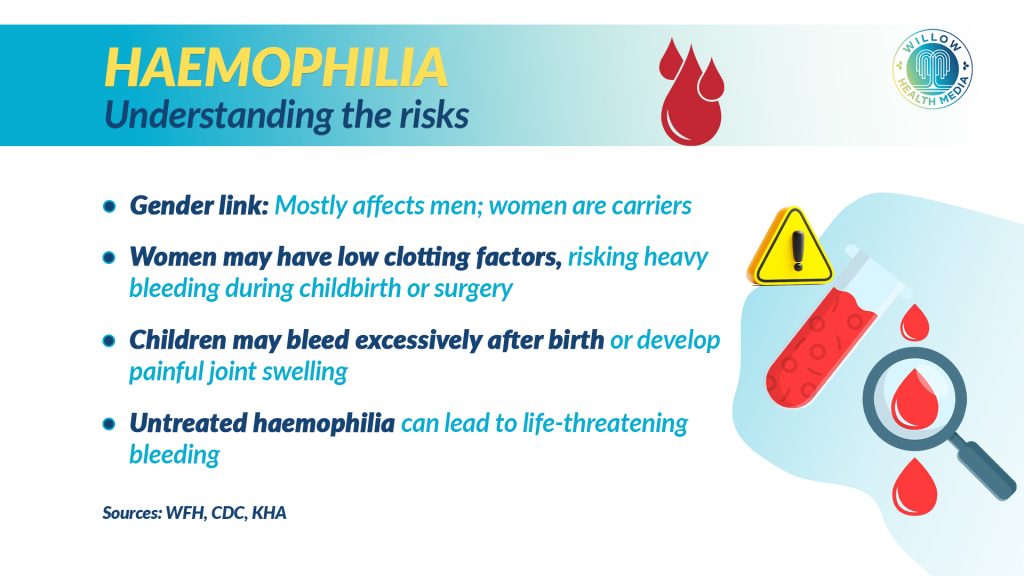
Dr Kibet explains that the condition is linked to the X chromosome. Since women have two X chromosomes, a healthy one can compensate for the faulty one. Men, however, only have a single X, which makes them more vulnerable.
There are three known types of haemophilia:
Type A – Factor 8 deficiency (the most common in Kenya)
Type B – Factor 9 deficiency
Type C – Factor 11 deficiency (very rare)
Children born with haemophilia may bleed excessively after birth, from injections, or develop painful joint swelling as they start crawling.
The biggest challenge? Late diagnosis. Many hospitals in Kenya still lack the capacity to test for haemophilia.
Treatment is available through plasma, clotting factor concentrates, or fast-acting injections, but the cost is staggering. A single dose for a child costs about Ksh75,000, while adults may need up to Ksh200,000 per treatment.
Dr Kibet adds that women, often silent carriers, face unique risks, especially during childbirth, and tragically, some lose their lives unnoticed.
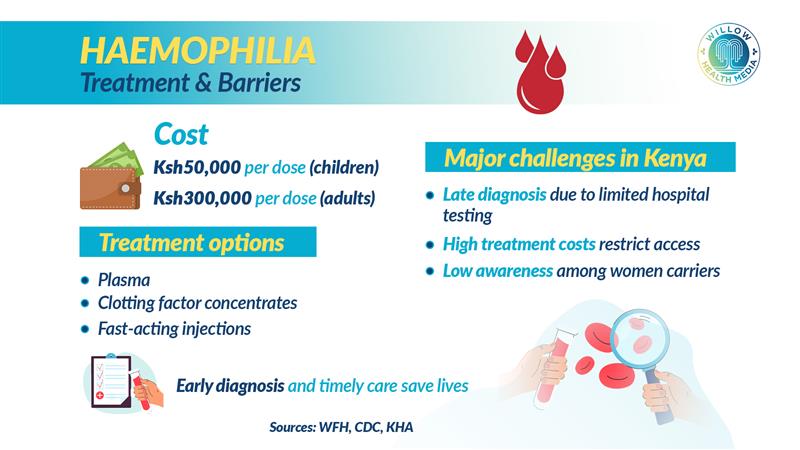
Haemophilia may be rare, but it is deadly. Awareness is the first step. Early diagnosis means timely care, and timely care saves lives.

This article, “Silence to Strength: Kenya’s haemophilia patients defy the odds with courage” offers vivid personal stories of Kenyans living with haemophilia, detailing obstacles like late diagnosis, high treatment costs, insurance exclusion, and reliance on donor supply.
It shows how stigma, misdiagnosis, and limited care leave families stretched thin and often on their own.
It’s a glimpse into the human reality behind the condition, and why understanding haemophilia goes beyond medical terms.




















