According to recent government data, two in five HIV infections happen among 15 to 24-year-olds, numbers pointing to the true scale of the crisis
At the beginning of this year, Kenya had made remarkable progress in HIV screening, with 96 per cent of People Living with HIV (PLHIV) aware of their status. About 98 per cent of those diagnosed with HIV were on anti-retroviral treatment, the majority of whom were virally suppressed, surpassing the global UNAIDS target of 95 per cent.
With such gains, Kenya is set to reap clinical and economic benefits. Not only is there likely to be a reduction in HIV- related morbidity and mortality, but the lower spread of HIV will probably result in savings on lifetime cost of medicine, reduced cost of HIV prevention measures, and decreased demands on the country’s healthcare system.
Globally, the landscape of pre-exposure prophylaxis (PrEP) and antiretroviral drugs (ARVs) is changing with the landmark innovations of long-acting formulations.
For instance, the injectable cabotegravir was found to reduce HIV risk by 89 per cent as compared to daily oral PrEP.
These are game changers in the quest for a HIV vaccine as they hold promise of accelerating HIV prevention and alleviating the psychosocial effects associated with daily intake of medication.
Another notable advancement in the field is HIV cure research. The past year saw the conclusion of a groundbreaking HIV cure trial, the first to be conducted in Africa. Considering Africa bears the largest brunt of HIV, the significance of this cannot be overstated.
So far, about 10 individuals have been functionally cured of HIV
Although this study was conducted in South Africa, the good news is there are HIV cure studies in the initiation stages in Kenya. Even more important is the fact that this is significant progress towards inclusion of data generated from communities that need a cure the most in informing design of therapies.
So far, about 10 individuals have been functionally cured of HIV. Functional cure means that the virus is suppressed without the need for medication.
The 10 underwent stem cell transplants, and while these are risky procedures which are not affordable and scalable, they provide important insights on what design of a cure would entail. It is evident that a cure may involve more than one strategy, and the various advances in research must be applauded.
At country level, while a 75 per cent reduction in HIV infections has been achieved, there exists a worrying trend among the youth.
According to government data, two in five HIV infections happen among 15 to 24-year-olds. These figures should concern us all and compel a rethinking into the ways the youth are engaged on HIV related matters, granted that this demographic are the key drivers of Kenya’s economy.
Consequently, it is important to invest in their wellbeing to ensure they remain healthy and productive. Furthermore, the Ministry of Health and other partners should leverage technology and incorporate innovative channels of communication such as social media so as to reach wider, younger audiences. Such age-specific strategies are progressive instruments for social behaviour change.
Kenya’s readiness was put to the test by US government funding freezes earlier this year
Indeed, the civil society and community- led organizations have been at the heart of Kenya’s HIV response. The significant strides made were a result of strong advocacy for the rights of PLHIV.
Concerted lobbying at country and global level saw formation of public private partnerships that resulted in increased access and availability of ARVs as well as effective deployment of HIV prevention strategies. It is important to note that the country’s HIV programming was heavily donor dependent.
While efforts were being made to institute self- reliance and sustainability, Kenya’s readiness was put to the test by the United States government funding freezes earlier this year.
Whereas the world is yet to fully comprehend the impact of the US funding cuts on HIV, it is however clear that it exposed the fragility of the HIV response in most low- and middle-income countries.
The adoption of the America First Global Health Strategy has exposed glaring vulnerabilities in HIV prevention services, HIV testing, viral load monitoring, human rights programming and community-led activities. It is important to note that the reduction in US funding, although abrupt, was a clear indication of the trend in reduction of all donor funding in HIV and health.
The decision by the US government not to commemorate this year’s World AIDS Day is yet another reminder of the great need to look inwardly for sustainable health solutions. Kenya must reduce overdependence on northern partners and realise that the solutions lie within.
A crucial step in ensuring sustainability of the HIV response is advocacy
There is political goodwill to ensure Kenya does not regress in the gains made against HIV. The Primary Health Care Act 2023 provides the framework for delivery of preventive medicine. Kenya spends 4.33 per cent of its GDP on health and 0.8 per cent of GDP in research against the 2 per cent stipulated in the Science Technology and Innovation Act.
A crucial step in ensuring sustainability of the HIV response will be advocacy to ensure the country’s commitments to health match the actual investment.
There is need for current monitoring of data coupled with locally generated scientific findings to guide advocacy, planning and financing of Kenya’s health priorities.
This means strengthening both health management information systems and local research.
Fortunately, research institutions, government, and academia have significantly developed their infrastructure and human resources through bilateral donor funding over the years. The question then is, how do we utilise this capacity to sustain the gains made in HIV, and leverage platforms initially used for HIV research to curb emerging and re-emerging diseases?
How do we utilise existing networks and partnerships to push multiple agendas towards a healthier vibrant society? One example is a recent meeting by the Global Gene Therapy Initiative and HIV Cure Africa Acceleration Partnership bringing together stakeholders from HIV cure and Sickle cell disease fields from across Africa to explore ways to advocate for gene therapy in Africa.
Such strategies highlight how Kenya can increase demand for specific therapies with the foresight of how other public measures can benefit in future, thereby increasing sustainability.
There is an opportunity for Africa to negotiate with pharmaceuticals for lower prices
New therapies such as long-acting PrEP present the challenge of limited affordability and access in Africa. For instance, the current cost of Ksh3.6 million per person per year makes wide scale roll out of Lenacapavir virtually impossible. There is however an opportunity for African regional economic communities to negotiate with pharmaceutical industries for lower prices.
Considering this is the region that is most affected by the HIV pandemic globally (20.8 million PLHIV), there are economies of scale that offer the region a strategic advantage. For instance, the cost of Lenacapavir could be brought down to about Ksh3,300 annually with an assured demand of 5-10 million people.
However, to ensure sustainability, Kenya needs to create an enabling environment for industry and pharmaceutical companies to manufacture such drugs and essential commodities.
This would not only cushion the country from effects of global shocks but would also help alleviate supply chain challenges.
Finally, the voice of the community remains critical in the realisation of an end to HIV. Moses Super Charger, a Ugandan advocate for PLHIV, gives a clear example of what innovation without the end users can result in.
Among the earlier ARVs brought to East Africa was a protease inhibitor which needed refrigeration. It was a good product, however, failure to include African PLHIV in its creation resulted in poor uptake as majority of the intended beneficiaries did not have access to fridges.
Currently, there are efforts to involve the community at all levels of the HIV response. However, more needs to be done to ensure there is genuine co-creation, where community members are not involved to tick a box but rather as part of a practical solution with PLHIV at heart.
It is clear that concerted multisectoral and regional collaborations will safeguard gains made in the fight against HIV while ensuring no one is left behind. The onus is on us to rise up and build on the existing infrastructure, political goodwill, brilliant minds, vibrant research environment and dedicated community to end HIV. The solution lies within.
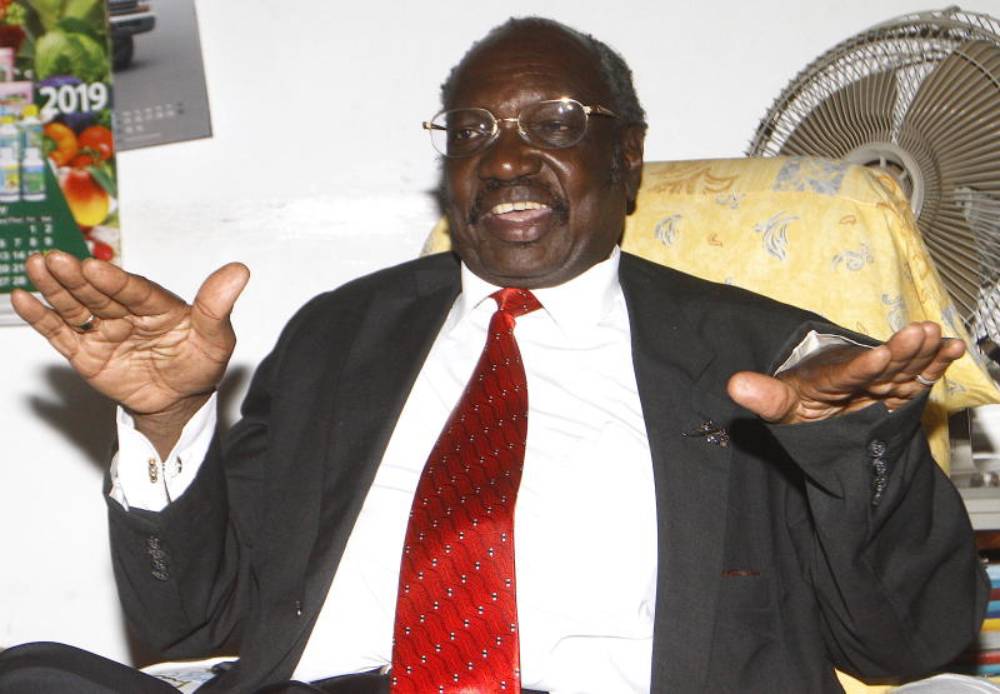
Dr Terry Muhomah is a research fellow in HIV cure and immunology at the University of Nairobi’s KAVI-Institute of Clinical Research