Babies born before 37 weeks are at higher risk of jaundice. So are those who don’t get enough breast milk. And if you notice pale-coloured stool, take it seriously—it’s often a red flag.
You might be taken aback to learn that repetitive lip-smacking, frequent blinking, and gazing blankly into space can be signs of subtle convulsions. These subtle convulsions often go unnoticed. Why? They are not very pronounced or can be mistaken for normal behaviour, like in Jane’s case, where she mistook repetitive lip-smacking for hunger.
Jane, a first-time mother to a six-day-old baby, barged into the paediatrician’s consultation room, looking wrung out and exhausted. She paced up and down like a cat on a hot tin roof. “My baby has been having frequent, weird cries, and has refused breastfeeding despite frequent lip-smacking. I am told his skin is more yellow compared to normal newborns.”
“Have you noticed the yellowness yourself?” asked the paediatrician.
“Not at all,” Jane replied.

“I am afraid we need to start phototherapy – a common treatment option for jaundice in newborns. The blue light helps transform bilirubin into forms that are easily eliminated from the body,” the paediatrician explained.
“We also need to run a few tests to determine the cause of the yellowness. Consequently, the lip-smacking which you mistook for hunger was likely several episodes of convulsions. Meaning, kernicterus has already set in. At this point, it is a situation of touch-and-go. It might result in death, and if the baby survives, be ready to bring up a child with disabilities.”
Unfortunately, the baby lost the battle to jaundice.
The mother’s immune system sees baby’s red blood cells as foreign
Kernicterus is brain damage in newborns caused by excess bilirubin (a yellow substance from red blood cell breakdown). Normally, the liver clears it out, but too much might cross into the brain, leading to damage and symptoms like uncontrolled body movements. Which can be subtle or obvious. As seen in Jane’s baby.
Who is at Risk?
Premature Babies: Those born before 37 complete weeks are prone to developing jaundice. Why? Their liver is not fully developed to clear bilirubin.
Blood Type Mismatch: If the mother’s blood type differs from the baby’s (such as in ABO or Rhesus incompatibility), her immune system may see the baby’s red blood cells as foreign. This triggers an immune response that destroys the baby’s red blood cells, causing a buildup of bilirubin in the blood. The result is newborn jaundice.
Neonatal Scalp Bruising: Bruising during birth, especially with vacuum-assisted delivery, can cause increased breakdown of red blood cells. This raises bilirubin levels in the baby’s blood, leading to jaundice. A visible bruise after a vaginal delivery should be seen as a potential warning sign.
Breastfeeding difficulties: When a baby doesn’t get enough breast milk, it can lead to dehydration and reduced elimination of bilirubin. This causes bilirubin to build up in the blood, resulting in jaundice.
Family History: If older siblings experienced jaundice, the newborn has a higher risk of developing it as well.
Baby boys: Male newborns are more prone to jaundice, often due to slower liver maturity and certain genetic factors.
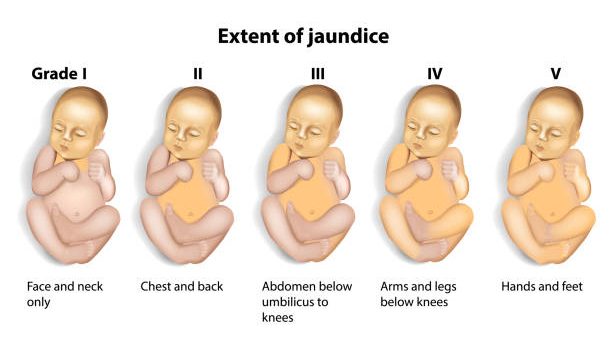
Yellowing starts on the face, moves down the body, and may affect the eyes
One life lost is one too many. Jane’s baby died from severe jaundice. Other serious complications can include:
Cerebral palsy: Kernicterus leads to cerebral palsy, leading to stiffness or uncontrolled body movements.
Hearing loss: High levels of bilirubin damage hearing nerves, leading to deafness and communication challenges.
Vision problems: High bilirubin levels can damage the optic nerve development, rendering one blind.
Intellectual Disabilities: High bilirubin can affect brain development, leading to learning and thinking difficulties.
If Jane had known how to check for jaundice, she wouldn’t have lost her child. Here are easy ways to spot jaundice.
Yellow skin: Starts on the face and moves down the body.
Yellow eyes: The white of the eyes look yellow.
Yellow inside the mouth: Especially the gums and roof of the mouth.
Dark yellow urine: Instead of clear to pale yellow urine.
Pale poop: It is a direct pointer to liver or bile duct problems and usually appears alongside jaundice. Therefore, watch your baby’s stool color carefully.
How to prevent newborn jaundice
Frequent feeding: Feeding 8-12 times a day helps eliminate bilirubin through stool and urine.
Timely C-section: Can prevent scalp bruising that may lead to jaundice.
If jaundice has already set in, it’s prudent to visit the hospital for phototherapy or exchange transfusion (replacement of baby’s blood to quickly reduce bilirubin) when phototherapy is insufficient.
Check Early, Check Often: Mothers should frequently check the white of the eyes, gums, and palate every 12 hours for signs of jaundice.
In Kenya, neonatal jaundice is among the leading causes of hospital admissions. Despite its prevalence, there is no reliable data on how many babies under 28 days old develop jaundice—or how many die from it. This gap is largely due to challenges in data collection.
Contributory factors include:
- Limited laboratory access: Unreachable bilirubin testing, thus missed diagnosis and documentation.
- Inadequate Skilled Staff: In some Kenyan hospitals, a single nurse may be responsible for over 20 newborns. This heavy workload often leaves little time to document jaundice cases—unless the condition results in death.
- Low Community Awareness and Ignorance: Mild jaundice is often overlooked by mothers or caregivers, leading to delayed hospital visits—sometimes after the baby is over 28 days old—or no visit at all. This delays care and makes accurate classification difficult.
- Weak Health Information Systems: Poor infrastructure and processes lead to inconsistent record-keeping and underreporting of jaundice cases.
- High Rates of Home Deliveries and Early Discharge: Many jaundice cases go unrecorded as they occur outside health facilities or do not receive medical attention at all.
To bridge these gaps in Kenya, there is a pressing need to increase staffing, provide targeted training, raise community awareness on neonatal jaundice, and strengthen health information systems.
In conclusion, mothers of newborns must remain vigilant. Watch closely for any yellowing in the whites of the baby’s eyes—don’t wait for it to spread. Even a faint tinge is a loud warning. Neonatal jaundice may appear mild, but if ignored, it can quickly turn fatal.
Jane’s baby didn’t survive. Had he lived, he might have faced cerebral palsy, hearing loss, or permanent disability. The tragedy is that this was preventable. With early detection and timely treatment—especially phototherapy—these outcomes can be avoided.
Neonatal jaundice is silent, but deadly. Act fast. It spares no soul.
Dr Rachel Kerubo is the Resident Medical Officer – Department of Internal Medicine, Nyamira County Referral Hospital.