The country has a shortage of 200,000 units of blood annually, resulting in seven out of 10 transfusions relying on blood from desperate families and friends—not safe, screened donors. Every delay risks lives. Every shortage spreads fear.
Edward Kwach, a renowned Kenyan radio host, passed away while undergoing treatment for meningitis at Nairobi’s Coptic Hospital on April 28, 2025. In the weeks leading up to his death, his family and friends made public appeals for blood donations to help stabilise his critically low iron and haemoglobin levels.
His was not an isolated case. Across the country, maternal deaths, trauma fatalities, and surgical complications often result from one common factor—the unavailability of safe, sufficient blood.
Then there was Jane Adhiambo, a mother of three (two with sickle cell disease) from Migori, who in September 2020 carried her 12-year-old Elvis to four hospitals at night, begging for blood. She got just one of the three units he needed.
Medics are not spared either. A nurse named Caroline was involved in a traffic accident in January 2022 while returning home from work in Kisumu County. She sustained severe internal injuries and significant blood loss, requiring an urgent transfusion. Tragically, the hospital faced a critical shortage and could not provide the blood needed. She died due to excessive blood loss, sparking national outrage and highlighting the urgent need to boost blood donation nationwide.
Blood samples sent over 360 km to Eldoret for testing, causing deadly delays
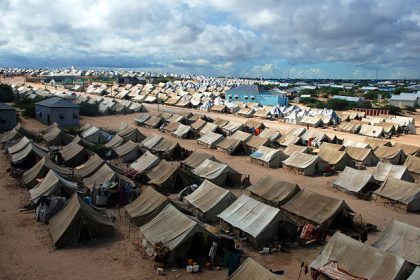
Most hospitals in Kenya face serious challenges with blood supply. Lodwar County Referral Hospital in Turkana earned the region the label of a “blood desert” from the Guardian in April 2024. It struggled to meet transfusion demands for its over 400 daily patients and referrals from 282 smaller facilities. Up to 75 percent of clinical blood demand goes unmet—so obstetric, trauma, and surgical patients can bleed out waiting for units to arrive. Indeed, blood samples had to be sent over 360 km to Eldoret for testing, causing deadly delays.
While maternal mortality remains high at about 342 deaths per 100,000 live births, with hemorrhage topping the list as a leading cause, WHO estimates suggest that timely blood access could reduce maternal deaths globally by 20 percent—a figure relevant for Kenya’s health goals.
Kisumu’s Jaramogi Oginga Odinga Teaching and Referral Hospital, has a storage capacity of 5,000 units but held less than 400 units in 2024, forcing patients to rely on relatives for donations that were often insufficient, leading to postponed surgeries and compromised care.
A 2020 study by Omutere and Abantanga titled, Assessing the Appropriateness of Blood Transfusion Among Injured Patients, indicates that voluntary, non-remunerated blood donation in Kenya is low, with many donations coming from family replacement donors, which impacts the safety and availability of blood.
Kenya previously relied on paid and replacement donors, increasing risk of transfusion-transmissible infections
The Kenyan National Blood Transfusion Service (KNBTS) faces a major blood supply shortfall, impacting maternal health, trauma cases, and chronic disease management, its 2021 Annual Report reveals.
Founded in 1984, KNBTS was tasked with ensuring a safe, adequate, and sustainable blood supply nationwide. Initially operating through regional centres, it later shifted focus to voluntary, unpaid donations—adopting global best practices to enhance blood safety. Before KNBTS, Kenya depended mostly on paid and replacement donors, raising risks of transfusion-related infections and causing shortages during emergencies.
For years, KNBTS relied heavily on donor funding, with PEPFAR covering up to 80% of its budget. However, when this support ended in 2019, the service struggled with critical shortages—including blood bags, testing kits, and staff (only 25% of the required personnel remained). Outreach programs were cut back, and key infrastructure, such as cold storage, deteriorated.
The current funding gap is estimated at Ksh500 million annually to fully cover all planned activities.
Despite efforts to phase out replacement donations, about 70-80 per cent of blood still comes from relatives or friends of patients, notes KNBTS. This reliance increases the risk of transfusion-related infections and compromises WHO safety standards.
Kenya’s voluntary blood donation rate remains below the WHO-recommended threshold of 15 donations per 1,000 people; current rates are about four to six donations per 1,000 population. This translates into a national deficit of approximately 200,000 units annually, with rural and marginalized communities contributing less than 30 percent of all donations. Dependence on school-based donation drives, which are seasonal and inconsistent, is also a major concern because when schools are closed, the supply drops significantly.
Many Kenyans believe donating blood causes weakness, illnesses or spiritual harm
Maintaining a cold chain across Kenya’s diverse geography, especially in arid and remote regions, remains challenging. Over 35 percent of blood transportation times exceed optimal durations, risking spoilage and wastage.
There have been alarming reports of illegal blood sales, with some hospitals charging patients for blood that should be free and bribery cases where patients or their families are asked to pay for access to blood.
Many Kenyans harbour myths—believing that donating blood causes weakness, illnesses, or spiritual harm. Fear of pain and social stigma also discourages potential donors.
Devolution has led to decentralization, but blood services often remain under central control. This disconnect hampers local mobilization efforts and creates logistical hurdles.
A 2021 study by KNBTS and Ministry of Health titled, Barriers to Voluntary Blood Donation in Kenya, singled out myths and cultural beliefs as major impediments to blood donation. The study, which surveyed youth and adults across urban and rural counties, found that widespread fears—including beliefs that blood donation can cause infertility, permanent weakness, or is spiritually taboo—contributed significantly to low donor turnout. It emphasized that community sensitization and debunking of myths are essential for improving blood supply sustainability in the country.
Training local health workers in blood collection, storage, and stock management
To close the funding gap, KNBTS is pushing for higher government funding—covering at least 70-80 percent of operational costs—while pursuing partnerships with pharmaceutical firms for reagents, which could cut expenses by up to 30 percent.
Modernizing testing equipment could boost blood screening efficiency from 80 percent to 98 percent, slashing transfusion risks. Expanding regional centres and upgrading cold storage systems may reduce wastage from 10 percent to three percent, saving around 200,000 units yearly. Introducing digital donor and inventory tracking systems could also improve responsiveness and curb stock-outs by 15-20 percent.
Clearer division of roles between national and county levels is essential, alongside better communication to resolve current structural overlaps. Training local health workers in blood collection, storage, and stock management—plus setting up regional hubs for centralized planning—would streamline blood screening and distribution.
A 2022 study on The Impact of Blood Campaigns using Mobile Blood Collection Drives on Blood Supply Management, at Prince Muhammad bin Nasser Hospital in Saudi Arabia revealed that mobile blood drives, community donor mobilization and education campaigns significantly boost donation rates. Kenya could adopt similar strategies by conducting regular voluntary blood drives in public spaces while implementing a recognition system, through certificates or community honours, to encourage repeat donors.
The approach should involve NGOs, faith groups and private sector partners to enhance reach and sustainability. Blood donation awareness must be integrated into community health talks using culturally appropriate messaging in local languages across suitable media platforms.
KNBTS requires Ksh1.2 billion annually to operate optimally, but only gets Ksh600–700 million
The 2020 report by the Centres for Disease Control and Prevention and the 2019 NHS Blood & Transplant report reveal that in many Western countries, over 70–90 per cent of blood donors are voluntary and unpaid—a key factor linked to high blood safety standards.
A 2006 study in the United States by George B. Schreiber, Convenience, Bane of Our Existence, and Other Barriers to Donation, highlighted the importance of regular donor retention programmes, incentives, and targeted campaigns to maintain a stable blood supply.
Currently, KNBTS requires about Ksh1.2 billion annually to operate optimally. However, government and partner funding stands at about Ksh600–700 million, leaving a 50 per cent shortfall. Closing this funding gap is essential for scaling initiatives, upgrading infrastructure, and expanding community outreach.
To effectively reduce blood shortages in Kenya, a successful strategy must integrate awareness campaigns, infrastructure development, management reforms, increased funding to KNBTS, and robust community engagement. These combined efforts will help ensure a sustainable, safe, and sufficient blood supply—ultimately saving lives and strengthening the nation’s healthcare system.
Dr Mutura Muchoka is Division Head, Special Programmes & Neglected Tropical Diseases Coordinator, Department of Health, Meru County.