The Phase 3 Trial of First TB Vaccine since 1921 involves over 20,000 participants and is ongoing in Kenya, Zambia, Malawi, South Africa and Indonesia.
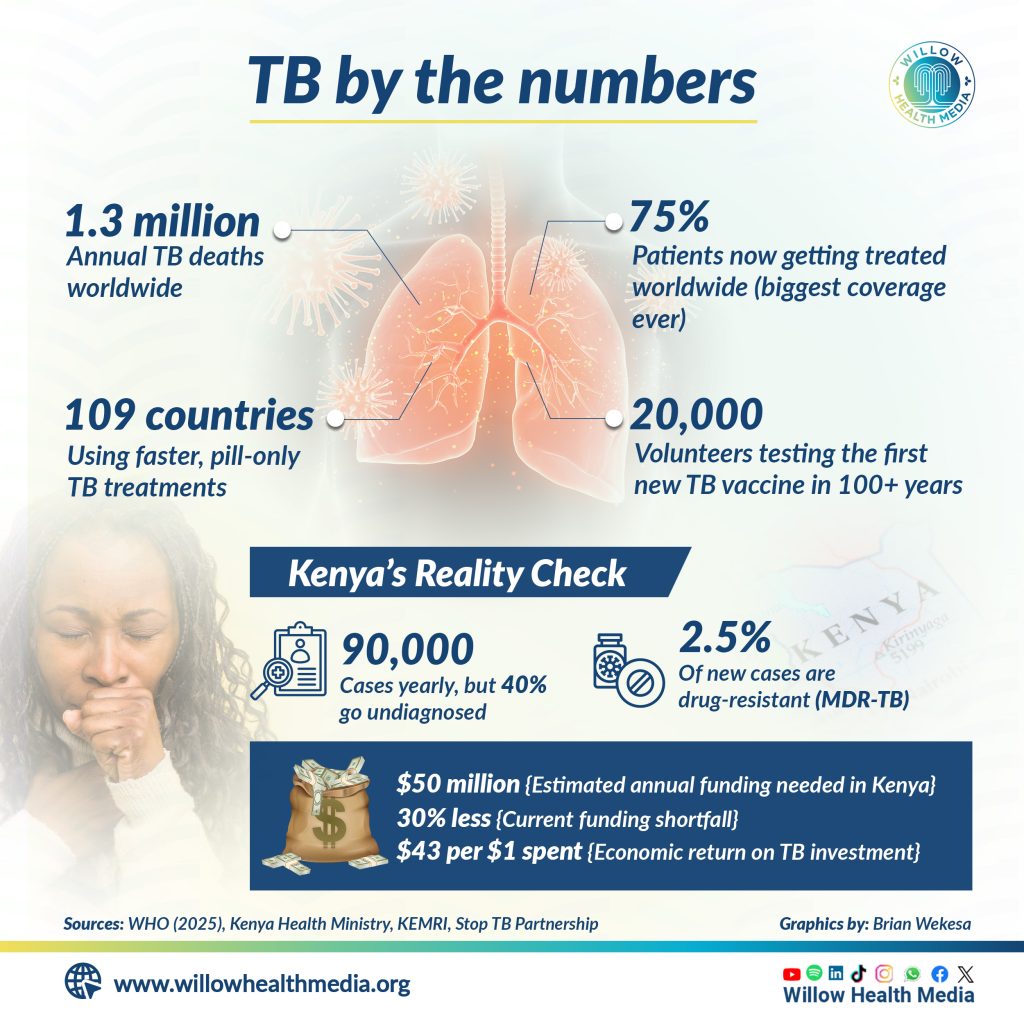
The fight against tuberculosis just hit a major win: 75 per cent global treatment coverage, the highest ever recorded, a major win over a disease that still kills 1.3 million people annually.
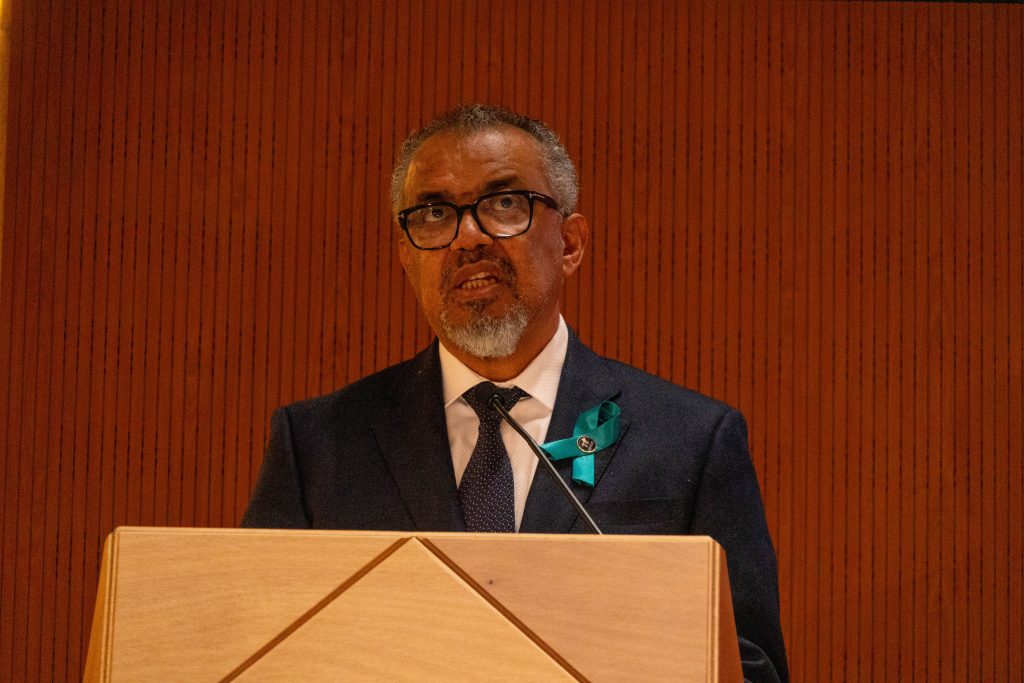
World Health Organization (WHO) Director-General Dr. Tedros Adhanom Ghebreyesus dropped the news during the 78th World Health Assembly (WHA) in Geneva, Switzerland.

The recent death of popular local DJ, MC Fullstop (John Maina) is a pointer to the devastation TB wreaks on patients.
While hospitalised, MC Fullstop posted on his Facebook page how one lung collapsed in 2021 with a Lung TB (Pulmonary Tuberculosis) diagnosis shortly thereafter.
The TB of the throat (Laryngeal Tuberculosis) in 2022 affected not only swallowing but also speech and mobility.
[Photo: Baba Talisha, Facebook]
Dr Tedros also said 109 countries have switched to the shorter, pill-only treatments for drug-resistant TB—no more painful injections, just higher cure rates.
And lurking in the labs is the ongoing Phase 3 trial of a new TB vaccine, the first of its kind in over 100 years.
With over 20,000 participants across South Africa, Kenya, Zambia, Malawi, and Indonesia, the vaccine could mark a turning point, and Dr Tedros reckons, “We are on the cusp of a breakthrough. This vaccine could transform TB prevention, especially in high-burden regions like Africa.”
Kenya, one of the 30 countries designated by WHO as high TB burden countries, has made commendable progress, although it still grapples with significant challenges.
According to the Ministry of Health, the country reports around 90,000 new TB cases each year, yet 40 per cent of these are either undiagnosed or unreported.

Multidrug-resistant TB (MDR-TB) represents 2.5 per cent of new cases, often necessitating expensive and prolonged treatment. While treatment success rates for drug-susceptible TB stand at a commendable 85 per cent, they drop to 60 per cent for MDR-TB due to treatment interruptions and drug side effects.
Earlier on, the Director-General of Health, Dr Patrick Amoth, reiterated Kenya’s determination to eliminate TB by 2030. “We’ve scaled up molecular diagnostics, expanded community-based testing, and introduced shorter TB regimens,” he said. “The ongoing vaccine trial in Kenya is a game-changer if successful, it will be a major tool in our elimination strategy.”
Kenya’s TB response is also being bolstered by technological and research innovations. The Ministry of Health has deployed AI-powered chest X-rays in Nairobi, Mombasa, and Kisumu to accelerate diagnosis and reduce human error. Additionally, mobile testing units introduced in informal settlements reached over 15,000 people in 2024 alone.
Research institutions such as the Kenya Medical Research Institute (KEMRI) are playing a vital role in the country’s TB strategy. KEMRI is currently engaged in local research to evaluate new TB drug combinations tailored for resistant strains.
However, Kenya’s ambitious TB control strategy faces a major obstacle: funding. According to WHO, an additional $5 billion is needed globally every year to achieve TB elimination targets.
Kenya, for its part, requires $50 million annually but is currently experiencing a 30 per cent shortfall in funding.
Dr Tedros stressed the urgent need for political commitment and financing, saying, “Investing in TB is not just a health imperative it’s an economic one. Every dollar spent on TB prevention yields $43 in economic returns.”
As the World Health Assembly continues, Dr Tedros and other global leaders are calling for increased domestic investment in TB programs, accelerated access to new vaccines and treatments, and stronger, more equitable health systems. Kenya’s progress is encouraging, but it underscores the need for sustained political will, community engagement, and global solidarity to end TB as a public health threat by 2030.
This story was first published by Willow Health Media on May 20, 2025






















