In the new guidelines, trained health professionals are mandated to begin comprehensive Post-Abortion Care with patient-centred counselling that is non-judgmental and non-stigmatising
Twelve years after withdrawing the Post-Abortion Care (PAC) guidelines, the Ministry of Health, albeit quietly, has released crucial new guidelines to healthcare providers who attend to women and girls alike in need of the often life-saving interventions.
Abortion in Kenya, like the rest of the world, is an emotive and controversial issue pitting religion, law and culture against each other, bringing up two conflicting sides: pro-choice and pro-life. But this binary lens of abortion is as myopic as it is misrepresentative of what abortion is.

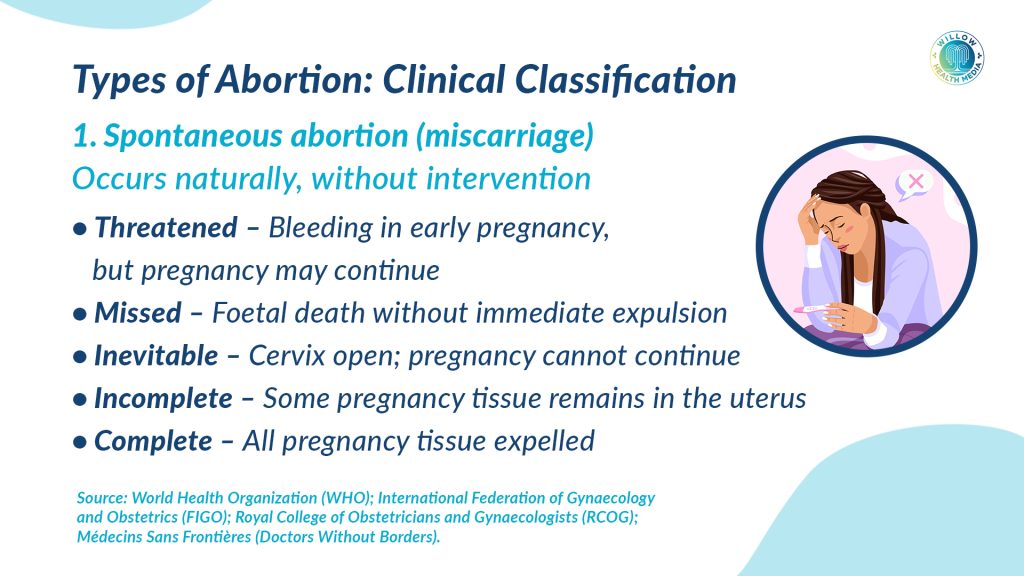
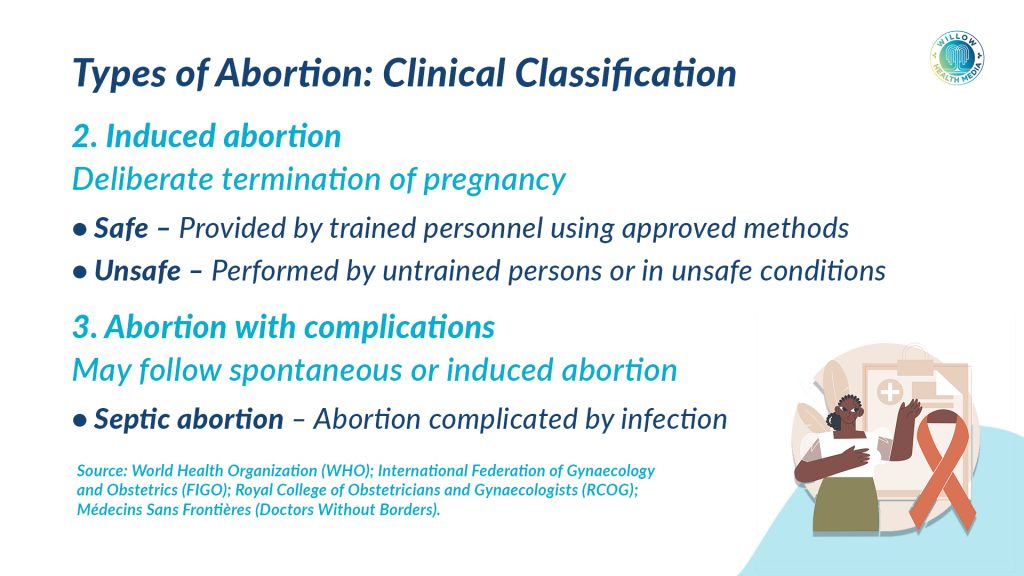
There are several types of abortion, commonly: missed, threatened, incomplete, and procured (safe or unsafe) abortions. The first three, also termed miscarriages, happen unprovoked due to chromosomal abnormalities, hormonal issues, uncontrolled diabetes, autoimmune disorders, uterine problems, infections and lifestyle factors like smoking.
The World Health Organisation (WHO) defines unsafe abortion as a procedure for terminating an unwanted pregnancy, either by people lacking the necessary skills, or in an environment lacking minimal medical standards, or both.
According to the International Federation of Gynaecology and Obstetrics (FIGO), unsafe abortions in Kenya are among the highest in Africa, accounting for about 17 per cent of the 6,000 maternal mortalities in the country annually.
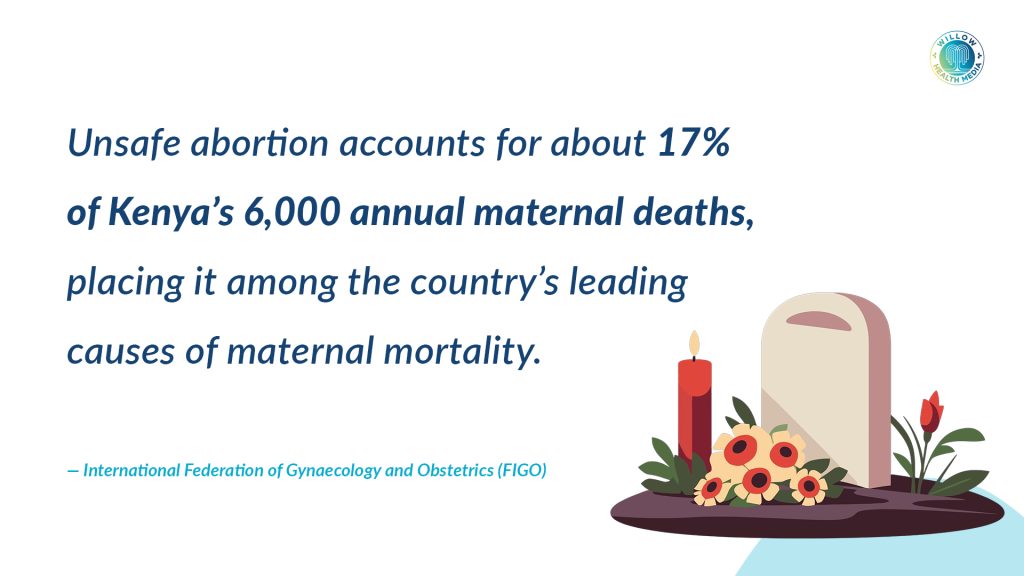
The Kenya Health Information System indicates that Post-Partum Haemorrhage is the leading cause of maternal mortality (40 per cent) and eclampsia (14 per cent). If this data is corroborated by FIGO statistics, it means unsafe abortion is the third leading cause of maternal deaths in Kenya.
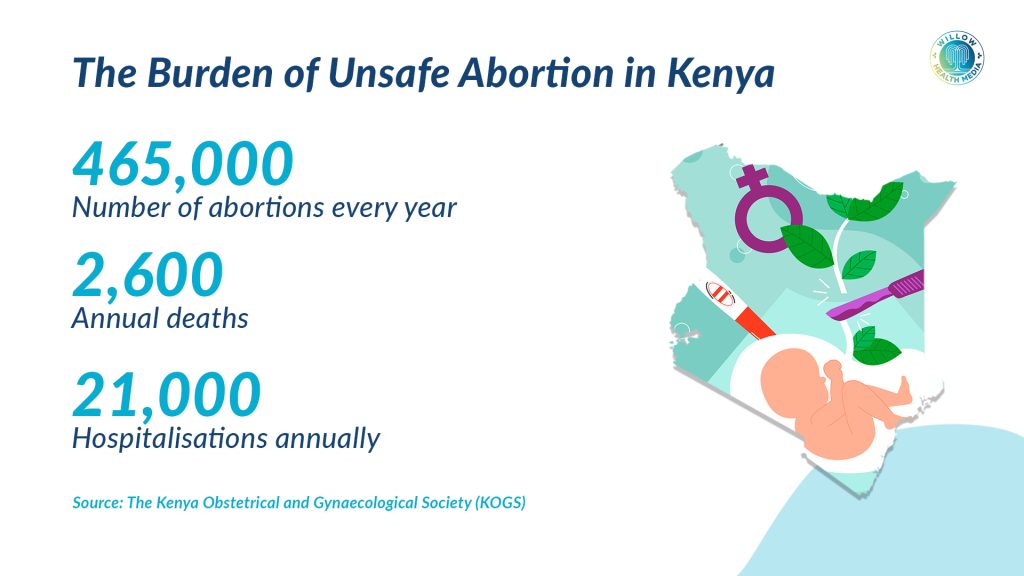
According to the Kenya Obstetrical and Gynaecological Society (KOGS), over 465,000 abortions occur in Kenya every year, with unsafe abortions linked to 2,600 deaths annually. KOGs records that another 21,000 women are hospitalised every year with complications from incomplete abortions, both spontaneous and induced.
Complications include excessive bleeding or infections arising from unsafe abortion
Globally, Doctors Without Borders indicates that one in six unintended pregnancies ends in abortion; while one in three of all pregnancies, both planned and unplanned, ends in an abortion. Globally, 45 per cent of all abortions are deemed unsafe as 29,000 women and girls die annually due to unsafe abortions.
Whether procured or spontaneous, women and girls presenting with complications from abortion need emergency care to save their lives. Complications include excessive bleeding or infections arising from unsafe abortion or retained products of conception after a miscarriage.

The May 2025 guidelines by the Ministry of Health address how to attend to mothers presenting in this state to not only attend to their immediate needs, but to also mitigate future similar situations. The guidelines first acknowledge that abortion-related complications contribute to Kenya’s maternal mortality rate of 355 deaths for every 100,000 livebirths.
“This underscores the urgent need for comprehensive, evidence-based interventions to manage incomplete abortion and its complications,” MOH Director General Dr Patrick Amoth states in the guidelines.
He describes PAC as a life-saving intervention for women who experience miscarriage and abortion complications. The handbook emphasises equipping frontline healthcare professionals to offer comprehensive counselling, manage incomplete abortions in time, offer post abortion contraception and family planning, and to manage other complications identified during PAC.
“Post-abortion care is an emergency service and, therefore, all women are entitled to have this service, offered in the confines of the law,” the guide states.
According to the handbook, PAC should be provided by trained healthcare professionals defined in the Health Act 17, part 1, as any person who has obtained health professional qualifications and is licensed by a relevant regulatory body.
In emergency cases, stabilising patients will be prioritised, but counselling must be done before discharge
The guide indicates that PAC should begin with mandatory comprehensive patient-centred, non-judgmental, and non-stigmatising counselling. Trained health professionals will be equipped to offer this service that touches on the physical, emotional and social impacts of abortion.
The prerequisites for PAC counselling include mental health needs assessment, a safe space to ensure privacy, use of two-way communication, and sign language. In emergency cases, stabilising patients will be prioritised, but counselling must be done before discharge.
The second stage of PAC provision is the management of incomplete abortion. At this stage, besides collecting the mother’s history, consent must be obtained from both adults and minors’ carers. Rhesus factor and tetanus status are among key items for examination at this stage, along with laboratory investigations for HIV and Sexually Transmitted Infections (STIs).
The handbook prescribes the use of Anti-D immunoglobulin injections for Rhesus-negative patients after abortion or miscarriage to avoid the formation of antibodies that could harm a Rhesus-positive baby in future.
It captures the management of severe vaginal bleeding, inspection of cervical injuries, and recommends the antibiotics to be used. Other management aspects provided for are shock, sepsis, retained products of conception, uterine perforation, intra-abdominal injury, genital injury, psychological and trauma management.
Another key component of the guide is the prevention of infection, where high level disinfection is prescribed. It underlines the implementation of evidence-based interventions like the prevention of unintended pregnancies through the use of contraception.
Community Health Promoters will be trained to give referrals and inform communities on Post-Abortion Care
The Ministry further recommends the establishment of rescue centres for those in pregnancy crisis, social protection for women with unintended pregnancies but who intend to carry their pregnancies to term.
To address the social challenges of abortion, the new guide calls for programs to reintegrate mothers back to society after miscarriages and abortion. While mothers with pre-existing reproductive conditions will be integrated to PAC, the guide also calls for the creation of community awareness on PAC and offering PAC services in public, private and faith-based facilities.
As things stand, the Catholic Church does not offer contraception and family planning services in their health facilities. Speaking to Willow Health, St Brigittas Eldoret Catholic Hospital Administrator, Sister Rosbella Kendagor, said Mission facilities compliment the government to offer healthcare services including free immunisation campaigns, “but we don’t offer family planning services.”
The PAC guide also recommends the establishment of youth-friendly health facilities and Sexual and Gender-Based Violence (SGBV) care. Community Health Promoters are set to be trained on PAC values to enable them to understand, give referrals and inform communities that PAC services are legal and available in all public, private and Faith-Based Organisations.
In a recent Kenya Quality of Care Health Facility service availability and readiness report, the assessment of Post-Abortion Care services showed that 21 per cent of facilities expected to offer PAC services were not providing them.
The 2023 survey by MOH showed that among primary-level facilities providing PAC, only 18 per cent could offer all the required components. Only 14 per cent of Level 2 and 31 per cent of Level 3 facilities could deliver basic components of PAC.
According to the survey, only eight per cent of private nonprofit or faith-based facilities and 14 per cent of public facilities could provide all basic PAC services.
The handbook directs parents or guardians with care orders over children to give consent for Post-Abortion Care
The legal foundation of the PAC guidelines stems from Article 43 (1) and (2) of the Constitution of Kenya, which state that every Kenyan has a right to access the highest attainable standards of healthcare, and that no Kenyan should be denied emergency medical treatment.
The publication of the PAC guidelines is anchored on Article 35 of the Constitution, which provides for the right to access information for the exercise or protection of other fundamental rights.
Addressing the possibility that minors would also need PAC services, the handbook directs parents or someone with care orders over children to give consent, in line with the Children Act No. 29 of 2022.
The current guide is inclined towards saving lives and taking advantage of opportunities to offer family planning and contraceptive counselling, along with linking women with reproductive health conditions to essential services.
The general misleading assumption that all abortions are procured highlights the importance of the PAC guideline. Before the promulgation of the Constitution of Kenya 2010, abortion was entirely criminalised. Currently, the law gives exceptions for abortion, “Where the life of the mother is in danger.”
The dilemma of adopting the exceptions in the new law emanates from the existence of sections 158 to 160 of the penal code which criminalise abortion. Section 158 criminalises individuals from attempting to procure an abortion for women lest they face a 14-year jail term.
Section 159 bars pregnant women from attempting to procure abortions for themselves, and Section 160 prohibits the supply or procurement of anything intended to be used unlawfully to conduct abortions. Breaching this attracts a jail term of three years.
On the other hand, Section 240 of the penal code indicates that one would not be criminally liable for performing surgery in good faith, with reasonable care and skill, for the patient’s benefit, or on an unborn child to save the mother’s life.
The PAC guide is an indicator that Kenya is learning from best practices in the UK, acknowledging that not all abortions are procured and that severe penalties are not a solution.


























