More than 2,000 people and 1,600 trucks cross the Busia and Malaba borders daily, stretching the disease surveillance system to full capacity
Kelvin Fredrick, 26, is a cybercafe operator at the Busia border point where he helps hundreds of travellers secure temporary passports daily. Kelvin contracted Mpox and suspects he caught the virus from dealing with the many cross-border travellers.
At first, Kelvin was treated for an allergic reaction at the Busia County Referral Hospital. But when the itchy rashes spread all over his body, along with swollen lymph nodes and fever, he was immediately admitted into the Alupe Sub-County Hospital isolation ward, where he’s still an inpatient.
Kenya has recorded 314 Mpox cases since the outbreak began in July 2024, with five deaths, and Busia County has emerged as a major hotspot, recording 63 confirmed cases and two deaths as of August 1. The county ranks second most affected in Kenya after Mombasa. At least 33 patients remain admitted in health facilities, 54 are under home-based care, and 222 have fully recovered, according to the Ministry of Health.
The World Health Organization announced a multi-country outbreak of Mpox in May this year. The highly infectious viral disease, caused by the monkeypox virus, began in the Democratic Republic of Congo before spreading to Kenya, Uganda, Tanzania, Rwanda, Burundi, South Sudan, Ethiopia, Malawi and Zambia.
It makes you weak, robs you of your appetite, and fills your body with painful sores. I wouldn’t wish it on anyone
Geoffrey Omuse, 64, from Kaukotoet village, also contracted the virus.

“At first, I thought it was just chicken pox,” says the father of eight. “The pimples started small, then grew bigger, the pain was unbearable, and I couldn’t sleep.”
His symptoms escalated to include fever, severe headache, muscle aches, fatigue and painful swelling. Laboratory tests confirmed Mpox, but surprisingly, none of his family members contracted the disease.
Although physically cured, Omuse says the mental and emotional scars linger.
“This disease is dangerous. It makes you weak, robs you of your appetite, and fills your body with painful sores. I wouldn’t wish it on anyone,” says Omuse.
Some patients experience more severe symptoms than the classic headache and painful blisters.

Peter Gakuru, 23, spent six weeks at Alupe Sub-County Hospital with large wounds oozing “a horrible-smelling fluid.”
His thigh began rotting from the inside, requiring surgery costing Ksh32,000, which was covered by his Social Health Insurance Fund.
According to the Centres for Disease Control and Prevention (CDC), Mpox Clade I causes more severe illness than Clade IIb, with fatality rates of 3–11 per cent. Clade IIb, linked to the 2022–2023 outbreak, had under 0.2 per cent fatality.
Jude Oduor, Manager at the Busia County Emergency and Operations Centre, said the two county deaths involved patients with underlying health conditions. HIV, diabetes, and hypertension significantly reduce survival chances when infected with Mpox.
Busia has an average daily crossing of 800–900 people and 1,000 trucks
“The most affected are aged between 25 and 45 years who are mainly cross-border traders, commercial sex workers, truck drivers, hawkers, and boutique operators,” Oduor said, attributing the rapid spread to the porous Kenya-Uganda border, where “people move in and out without being screened, which makes Mpox transmission within the community faster.”

Dr Susan Outa, County Chief Officer for Public Health and Sanitation, said Busia remains vulnerable due to high human traffic. “From Covid-19, Ebola to cholera and now Mpox, the trends show that we must stay ahead of emerging outbreaks.”
Busia has an average daily crossing of 800–900 people and 1,000 trucks, while Malaba records over 1,000 people and 600 trucks. Port health officers screen travellers at both border points.
The Kenya Revenue Authority collected Ksh879.33 billion from border points in 2024/2025—an 11.1 per cent increase. This marks a daily average of Ksh3.546 billion, making border closures economically costly.
Worldwide, 30,022 Mpox cases were confirmed across 79 countries between January 1 and June 30, according to WHO data. Of these, 119 people died, and 21 African countries reported ongoing transmission.
We are advocating for an emergency response fund to deal with future outbreaks
Kenya has screened 4.7 million travellers at airports and major entry points. The country’s first case in July 2024 involved a truck driver on the Northern Corridor. Of the first five cases, four were imported and one was locally transmitted.
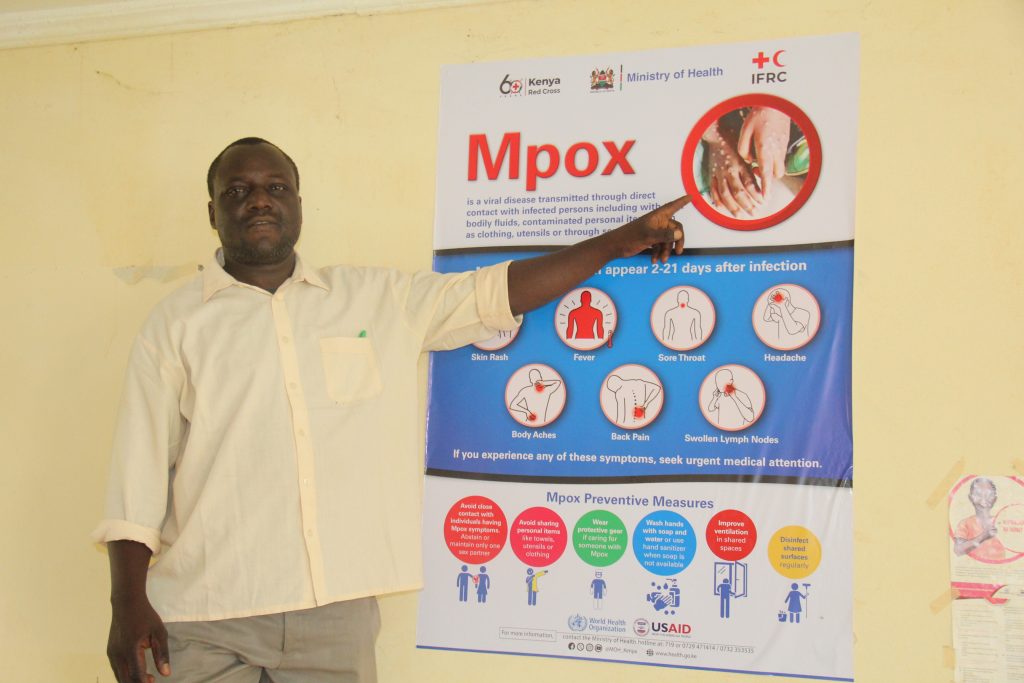
Busia operates with a Ksh2 million Mpox response budget, working with UNICEF, the Ministry of Health, and the Kenya Red Cross. However, the shortage of essential supplies remains a major challenge.
“To bridge the gap, we are advocating for the establishment of an emergency response fund to deal with future outbreaks,” Dr Outa says. “Given our location, Busia will always be at high risk, and residents must adopt routine preventive measures such as wearing masks, washing hands, and avoiding hugging or shaking hands.”
Busia County can test over 1,000 samples daily and supports testing for five neighbouring counties through its link to the National Public Health Laboratories.
Epidemiologist Valerian Karani emphasises strengthening surveillance systems. “If we can identify suspected cases quickly, trace their contacts effectively, and respond to alerts with urgency, we have a real chance of stopping Mpox in its tracks before it spreads deeper into communities.”
Kenya and 11 other African states signed a regional pact in May to strengthen surveillance, data-sharing, and resource pooling for Mpox control at border points.
Evans Shiraku, Busia disease surveillance coordinator, suggests vaccination campaigns for high-risk groups, including truck drivers, sex workers, and frequent cross-border travellers, could break transmission chains.





















