President Trump’s stop work order disrupted Kenya’s healthcare system, putting years of progress in HIV treatment, malaria prevention, and other vital services at risk
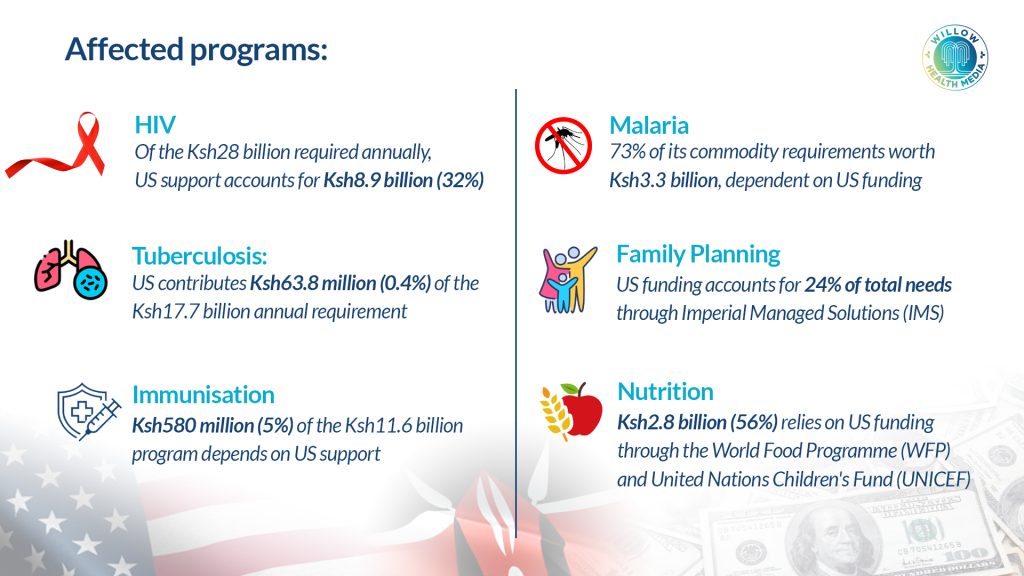
The withdrawal of foreign aid by the United States government has left Kenya with an annual financing gap of over Ksh78 billion in its health programs.
A comprehensive policy brief released by the Ministry of Health on March 10, this year, shows that the funding freeze started by US President Donald Trump early this year has affected health programs worth Ksh78 billion. This puts at risk the health and lives of millions of Kenyans who depend on donor-supported health services.
The crisis became clear when examining the financial breakdown of affected programs following Executive Order No. 14169 on January 20, 2025, which imposed a 90-day freeze on new US foreign development assistance.
The stop work order created a ripple effect across Kenya’s health system, threatening to reverse decades of progress in HIV treatment, malaria prevention, and other critical health interventions.
Of Kenya’s total health program requirement, approximately Ksh24.9 billion (31 per cent) comes from US government support for buying, storing, and distributing essential commodities.
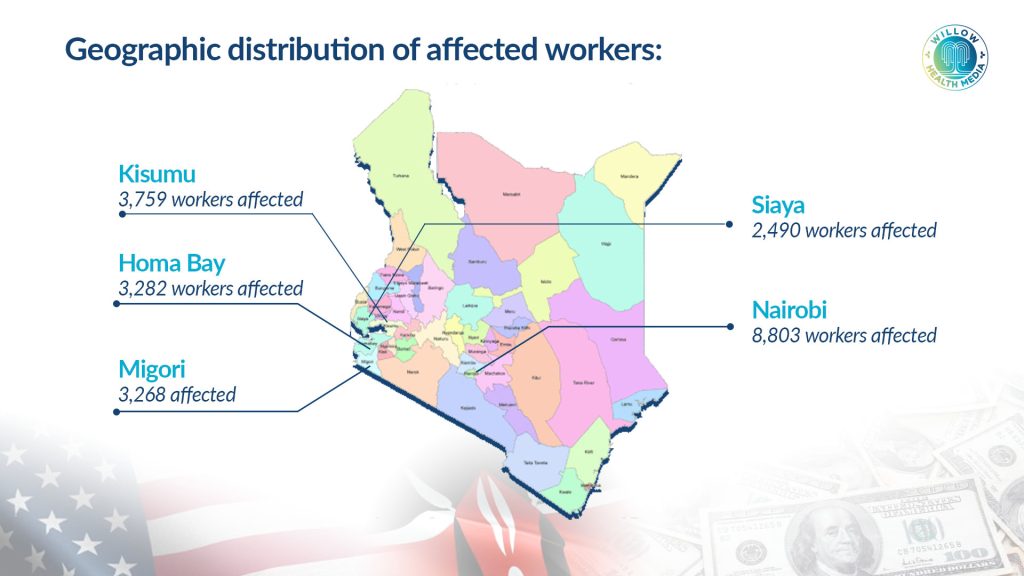
The human cost of the funding freeze has been severe. The policy brief reveals that 41,547 health workers supported by The US President’s Emergency Plan for AIDS Relief (PEPFAR) across all 47 counties have been affected, representing a total investment of Ksh17.38 billion annually.
Already, counties have reported the loss of 10,982 staff members, with the highest impact in Nairobi (8,803 workers), creating severe gaps in service delivery.
This workforce reduction directly impacts critical services including HIV prevention and treatment, TB control, malaria prevention, maternal and child health, immunisation programs, and emergency responses.
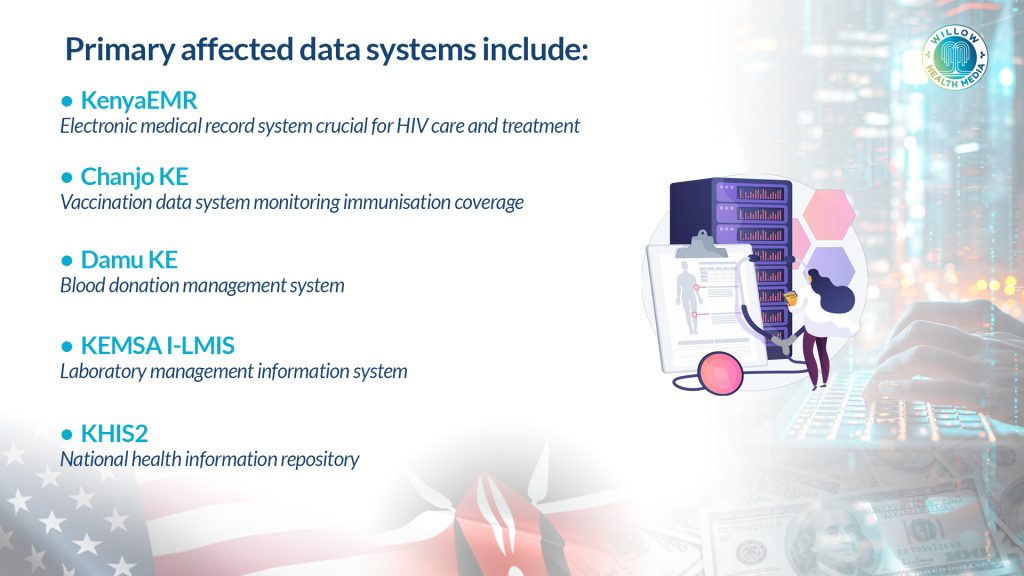
The funding freeze further threatens Kenya’s health information infrastructure, putting at risk key systems that form the backbone of health service delivery and decision-making.
The disruption creates multiple vulnerabilities such as infrastructure gaps due to lack of maintenance and technology updates, reduced training capacity for health personnel managing data systems, and increased cybersecurity risks as protective measures become underfunded.
Other risks include weakened disease surveillance affecting outbreak detection and response, delayed monitoring and evaluation of critical health programs, and persistent commodity shortages.
The stop work order created immediate shortages across multiple health commodity categories. For instance in the HIV program, despite a life-saving humanitarian assistance waiver being issued, there are still concerns about the long-term future of PEPFAR funding and reauthorisation.
The waiver allows for the continuation of services like antiretroviral medication distribution and prevention of mother-to-child transmission, but ARV stock levels are barely sufficient to carry the program through November 2025, creating uncertainty for 1.4 million people on antiretroviral treatment.
The funding freeze exposed critical vulnerabilities in Kenya’s health policy implementation
The malaria program is among the most severely affected, with 73 per cent of commodities managed through MEDS inaccessible. Critical impacts include over eight months of malaria rapid diagnostic test kits rendered inaccessible, five months’ supply of first-line medicines unavailable, and pregnant women losing access to routine bed nets and preventive medicines.
This is almost similar to the family planning program where commodities remain well below the required 15-month minimum, affecting over 6.2 million clients.
While representing only 0.4 per cent of commodity needs, the 69 per cent overall funding gap in the Tuberculosis (TB) program threatens long-term program viability. More significantly, the World Bank support towards blood services in Kenya ended in March, leaving the program with an urgent mobilisation need of over Ksh2.7 billion to prevent collapse.
The funding freeze further exposed critical vulnerabilities in Kenya’s health policy implementation, particularly affecting the rollout of the Social Health Insurance Fund (SHIF).
Key challenges include funding shortages hampering full implementation, disruptions to HIV treatment integration within broader healthcare coverage, administrative capacity concerns in managing the transition from government-subsidised to mixed public-private contribution models, and affordability issues for low-income populations previously supported by donor funding.
In response to the unfolding crisis, the US Government introduced several targeted waivers to reduce the crisis and provide temporary relief: Among these is the ‘Life-Saving Humanitarian Assistance Waiver’ issued January 28, 2025, which protects essential medicines, emergency medical care, and subsistence assistance.
Dependency on donor support has created systemic vulnerabilities that could increase maternal and infant mortality rates
Others are the ‘PEPFAR-Specific Waiver’ issued February 1, 2025, which continues HIV care, treatment, testing, and prevention services; the ‘Essential Administrative Costs Waiver’ which maintains salaries for key personnel in critical functions, and the ‘Pre-Pause Expense Reimbursement Waiver’ which enables recovery of legitimate expenses incurred before the freeze.
However, several critical programs lack waivers, including malaria prevention (73 per cent of needs), family planning (24 per cent of needs), and nutrition programs (56 per cent of needs).
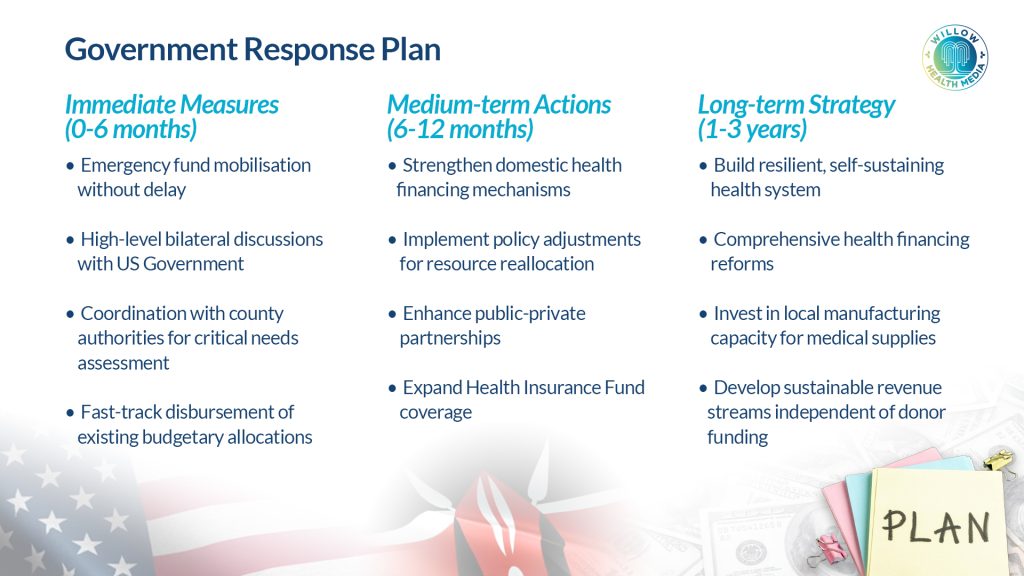
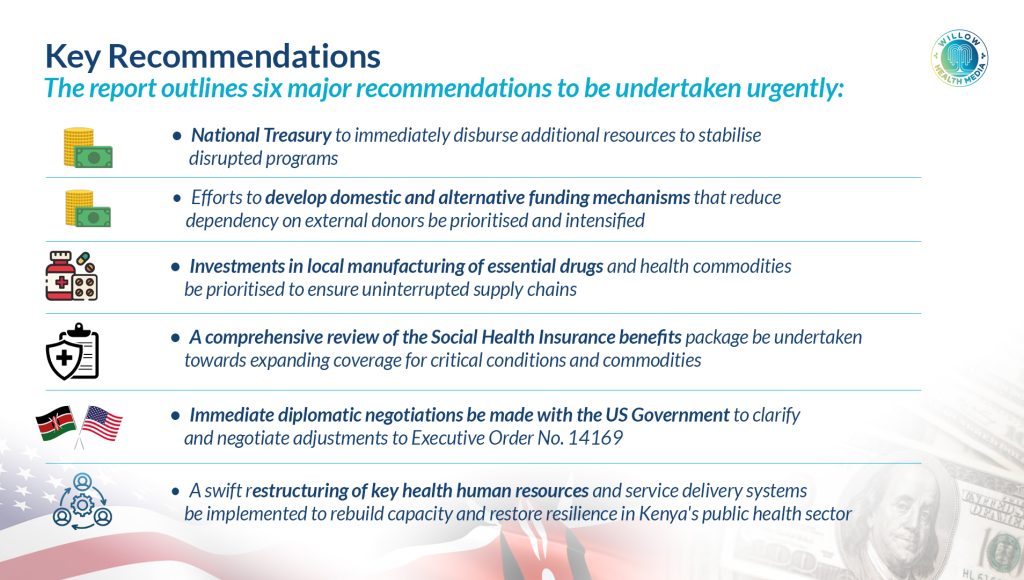
Similarly, Kenya’s Ministry of Health has outlined urgent recommendations for Cabinet action in three timelines namely immediate measures to be taken in six months, medium-term actions in the next 12 months, and a long-term strategy to be actioned in three years.
The aid withdrawal crisis extends beyond immediate health impacts. The report estimates the funding gap at Ksh28.4 billion, highlighting Kenya’s dangerous over-reliance on external donor support. This dependency has created systemic vulnerabilities that could increase maternal and infant mortality rates, reverse gains in HIV treatment coverage and trigger malaria outbreaks in endemic areas.
There are fears that it could also compromise immunisation coverage leading to vaccine-preventable disease outbreaks, and worsen malnutrition rates, particularly in arid and semi-arid regions.
The crisis, while devastating, presents an opportunity for Kenya to build a more resilient health system. Key priorities include diversifying funding sources through innovative financing mechanisms, strengthening domestic resource mobilisation for health and building local manufacturing capacity for essential medicines and supplies.
The Blood Services Program faces a critical shortfall of Ksh3.7 billion
The US stop work order represents the most significant threat to Kenya’s health system in decades. With over 41,000 health workers affected, critical commodities running short, and essential data systems at risk, the government faces an unprecedented challenge in maintaining health service delivery.
The crisis underscores the urgent need for Kenya to transition toward health system self-reliance while maintaining the quality and coverage of services that have saved millions of lives.
Already, one critical step was achieved after Kenya’s Ministry of Health received a record Ksh138.1 billion allocation in the 2025/26 budget – an 8.74 per cent increase from the previous year’s Ksh127 billion, making it the largest health budget boost in the country’s history. Of this, Ksh21.9 billion will go into the Global Fund to cover critical programs including HIV, TB, malaria, family planning, immunisation and vaccination.
However, the blood services program still faces a critical shortfall of Ksh3.7 billion after the government allocated a paltry Ksh300 million in the 2025/26 budget, leaving the Ksh3.7 billion deficit.
As the then Health Cabinet Secretary Dr Debra Mulongo Barasa noted, this is “a decisive moment for Kenya to consolidate successes and ensure healthcare accessibility regardless of external funding fluctuations.”
The coming months will be critical in determining whether Kenya can successfully navigate this crisis while preserving the hard-won gains in public health, particularly in HIV response.
Without immediate action, the report warns, millions of Kenyans face the prospect of reduced access to life-saving health services, potentially reversing decades of progress in the fight against HIV, malaria, TB, and other preventable diseases.





















