The nationwide closure exposed deep rot in healthcare, from unlicensed clinics to fake doctors breaking the law, leaving patients dangerously exposed.
Kenya’s medical landscape is undergoing a dramatic transformation as regulatory authorities intensify their crackdown on non-compliant healthcare facilities. The Kenya Medical Practitioners and Dentists Council (KMPDC) has launched an unprecedented nationwide enforcement drive, targeting clinics and hospitals failing to meet operational standards.
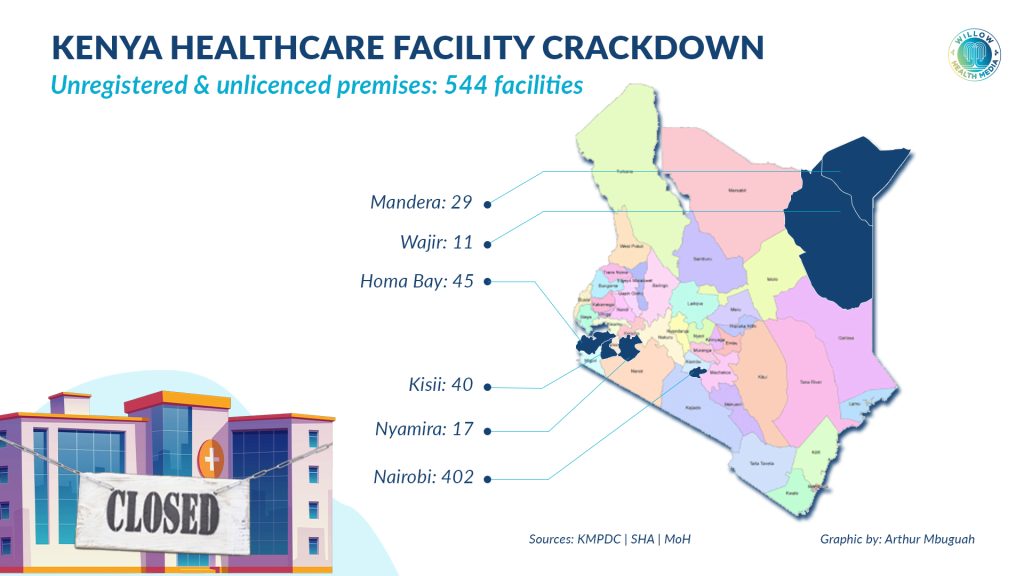
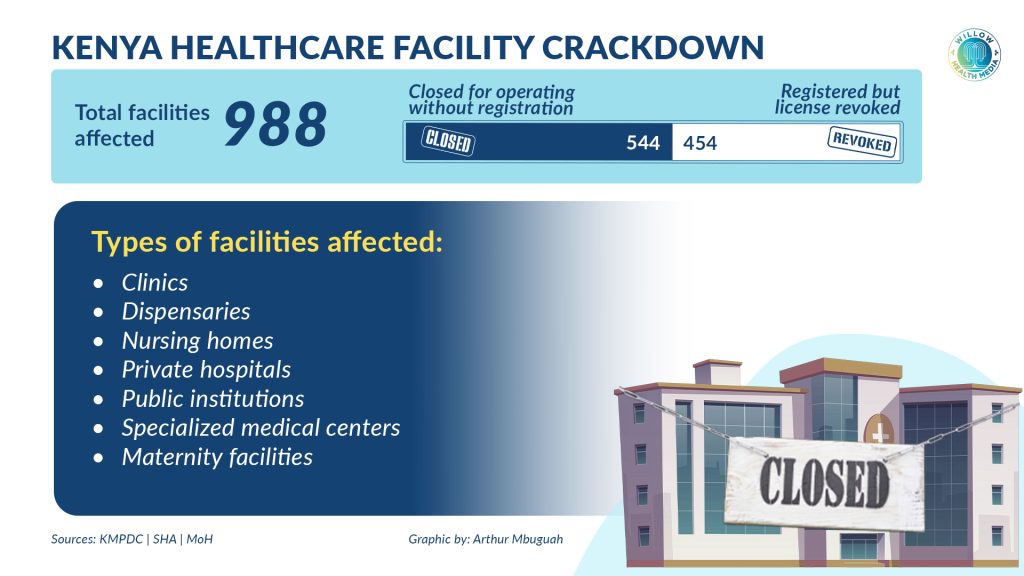
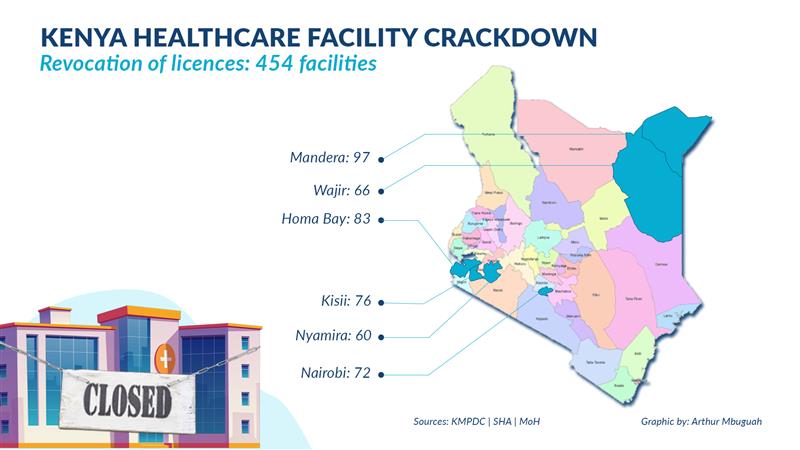
According to a Kenya Gazette notice dated August 29, 2025, a total of 544 facilities were closed for operating without proper registration. Additionally, 454 facilities had their licenses revoked due to serious breaches of medical standards and regulations. These measures affected clinics, dispensaries, nursing homes, and private hospitals across several counties, including Nairobi, Wajir, Mandera, Kisii, Nyamira, and Homa Bay.
In a phone interview with Willow Health Media, Dr David Kariuki, the KMPDC Chief Executive Officer, explained that facilities can also be closed even if they are registered.
“Those that are registered and licensed can also be closed for various reasons. One of the things we do is to ensure patient safety. A patient can only be safe if all the things required to treat them are available in a facility,” he said.

He cited key reasons for closures, including lack of proper infrastructure, inadequate human resources, poor waste management practices, missing standard operating procedures, and failure to ensure patient security.
“Depending on the level of non-conformity to the standards in the law, we can either close a section of a facility, revoke a license, or close the whole facility,” Dr Kariuki added.
“These 454 facilities were registered, but upon inspection, we found issues with human resources, waste management, and service delivery. When we register a facility, it’s a promise to maintain standards. If they fail to adhere, we give sanctions, which can include closure if patient safety is at risk,” Dr Kariuki explained.
He added that in most cases, facilities are given up to three months to correct non-conformities. “Those able to address the issues sooner can request a reinspection within the three months,” he said.
Of these closures, 402 facilities were in Nairobi alone, with Wajir recording 11 closures and Mandera 29, resulting in 544 establishments shut in just three counties. Separately, the Social Health Authority (SHA) suspended 45 health facilities across 16 counties, barring them from receiving benefits under the Social Health Insurance scheme.
The crackdown has revealed systematic violations across the healthcare sector. Many facilities were operating without proper health institution licences, violating provisions of the Medical Practitioners and Dentists Act, CAP 253. Others were employing medical practitioners or dentists who were not registered and licensed, contrary to professional standards.
KMPDC, in collaboration with other health regulatory bodies and county governments, has intensified nationwide enforcement of the Inspections and Licensing Rules.
Shut-down or downgraded facilities were unregistered, unlicensed, or operating below required standards
The CEO said a recent inspection of 288 health facilities in Nairobi led to the closure of 158 and the downgrading of 25, while 105 were allowed to continue operating at their current level.
Most of the facilities that were shut down or downgraded “were unregistered or unlicensed, had employed practitioners that were unregistered or unlicensed, or were operating below the required standards,” Dr Kariuki explained. “Others lacked critical infrastructure such as pharmacies, maternity wings, and laboratories. Some faced sanitation issues and inadequate waste disposal, which pose a direct threat to patient health.”
Dr Kariuki said enforcing the Inspections and Licensing Rules, 2022, was under the Medical Practitioners and Dentists Act, as “Our primary duty is to protect patients,” Dr Kariuki stressed. “We will continue to enforce these regulations firmly and fairly, so that every Kenyan receives the quality healthcare they deserve.”
To promote transparency, he said, KMPDC will gazette the names of all closed health facilities, encouraging patients to seek care only from compliant institutions.
“This information has also been shared with the National Government Administration Office, county governments, the Social Health Authority, the Digital Health Authority, and other health regulatory bodies to ensure continued compliance,” he added.
Suspended facilities include both private healthcare providers and public institutions
According to Kenya Gazette Notice No. 12003, SHA CEO Dr Mercy Mwangangi suspended facilities across 16 counties during their suspension period. Mandera leads with nine suspended facilities, representing 20 per cent of the total. Kisii follows with seven facilities (15.6 per cent), and Homa Bay with five facilities (11.1 per cent). These three counties together make up 46.7 per cent of all suspensions, pointing to localised compliance challenges in specific regions.
Among the suspended facilities are both private healthcare providers and public institutions, including two Equity Afia branches in Homa Bay and Mandera, indicating that the suspension cuts across different categories of healthcare providers.
The affected facilities range from specialised medical centres and nursing homes to maternity facilities and general hospitals. Notable suspended institutions include Rachuonyo East Sub-County Hospital, Nyanchwa Adventist Mission Hospital, and several private medical centres across the country.
Speaking at an earlier press conference, Health CS Aden Duale said that the government’s position on safeguarding public resources has been consistent, clear, and unwavering.
“Our commitment to an uncompromising stance against fraud is a foundational pillar of the Taifa Care programme. The concerns now being raised are not new; they have been an integral part of our public discourse and enforcement actions from the very beginning. We must ensure the prudent and accountable use of public funds, as mandated by the Public Finance Management Act. Every shilling contributed to the Social Health Insurance Fund must go towards legitimate, life-saving healthcare. On ensuring transparency and social accountability, we are committed to transparency,” the CS explained.
Hospitals that suffered closures to wait at least three months before appealing
The healthcare sector has recently faced scrutiny from multiple regulatory bodies. The crackdown, published in the Kenya Gazette on August 26, 2025, follows weeks of investigations into suspicious billing practices, including duplicated maternity claims, fabricated clinical records, and unqualified staff authorisations.
In a recent public notice by the KMPDC, the council clarified that hospitals that have recently suffered closures will have to wait at least three months before appealing. Similarly, any facility that wishes to update its assigned bed capacity must submit an official written request for inspection.
KMPDC’s mandate extends beyond simple licensing to ensuring that healthcare facilities meet minimum standards for patient safety and care quality.
The suspended facilities will need to address the issues that led to their suspension before they can be reinstated into the SHA network. The authority has not indicated the duration of the suspensions, suggesting they may be indefinite pending compliance with set requirements.
The SHA has not disclosed the specific reasons for the suspensions, though such actions typically follow compliance failures, quality concerns, or administrative irregularities identified during facility assessments.




















