Strict monitoring ensures facilities can move up or down in ranking- not just based on infrastructure, but on staff, equipment, and service quality
Kenya’s healthcare is a carefully organised, step-by-step network, designed to ensure citizens receive complete care from grassroots services to highly specialised national hospitals.
At the heart of this organisation is the Kenya Medical Practitioners and Dentists Council (KMPDC), the government body that, through its laws and policy guidelines, categorises and oversees health facilities across the country.
“In Kenya, we categorise health facilities from Level 1 to Level 6 based on Ministry of Health policy guidelines, the Kenya Essential Package for Health and the Strategic Plans,” explains Dr David Kariuki, the CEO of KMPDC.
“And once that is done, we regulate each level under the Health Institutions Rules gazetted in 2021.”
The foundation of this categorisation depends on three main pillars: the level of skill of the staff, the infrastructure (buildings and equipment) available, and the range of additional services offered.
The foundation of Kenya’s healthcare system is formed by Level 1 facilities called Community Health Units (CHUs).
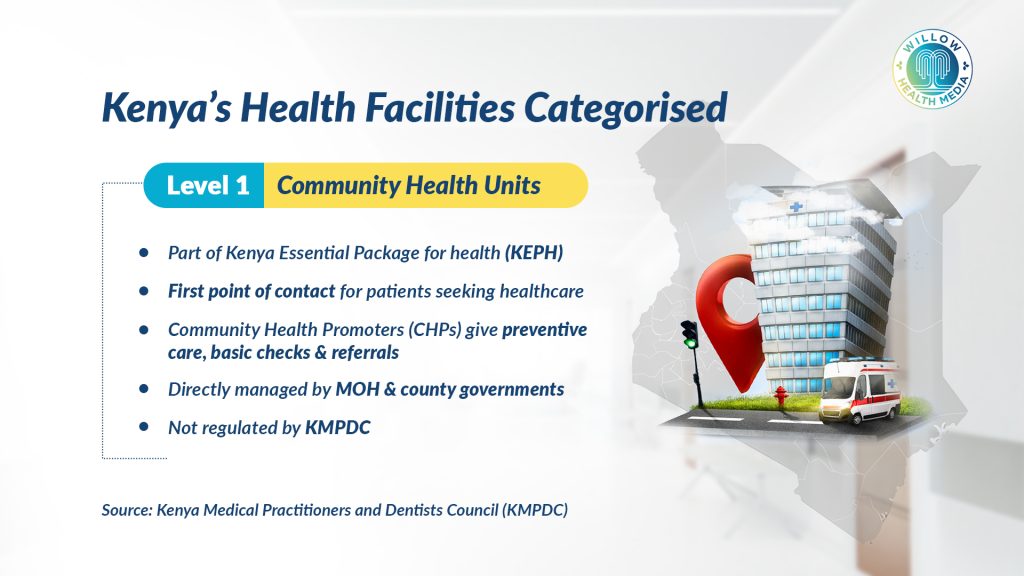
“These are not directly regulated by the KMPDC as they are services one can receive in their house and they are part of Kenya Essential Package for Health and are directly managed by the Ministry and the county governments,” explains Dr David Kariuki.
These units operate within communities, staffed by Community Health Promoters (CHPs) who report to Community Health Extension Workers (CHEWs) who are basically nurses or public health officers in the Level 2 facilities, although not in all the facilities.
They focus mainly on preventing disease, promoting health, and serving as the vital first point of contact between households and the formal healthcare system.
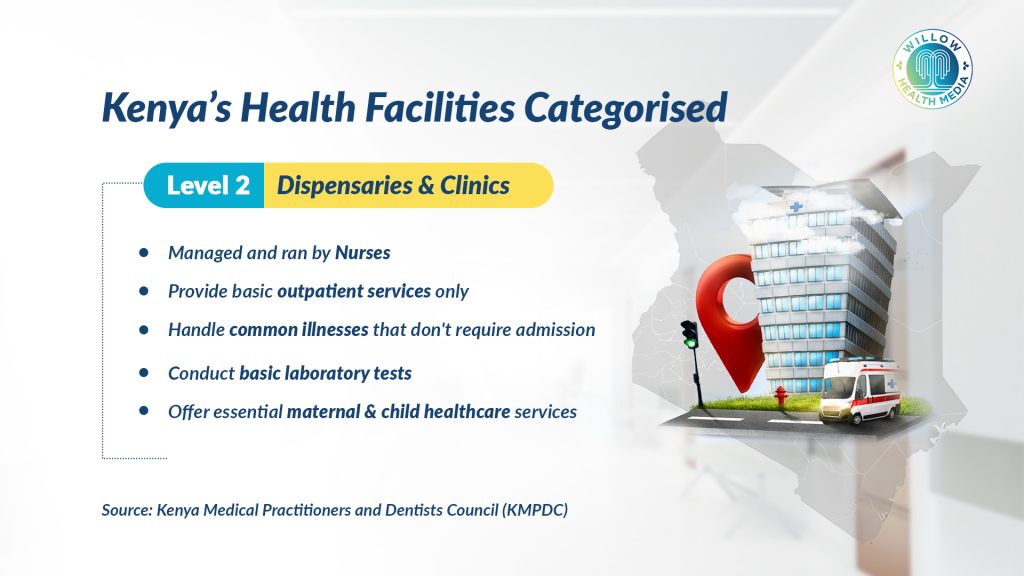
Moving up the ladder, the levels are distinguished by increasing medical expertise and facility capabilities. Level 2 healthcare facilities are categorised as dispensaries and clinics.
“One of the key things is human resources, in that what is the highest level of skill that the facility will have, and if the highest level of skill is a nurse, that means it is the most basic service that can be provided,” Dr Kariuki states.
These facilities, which form the most basic point of contact for common illnesses, provide basic outpatient services (treating patients who don’t need to stay overnight), essential maternal and child healthcare, and minor laboratory tests. They typically don’t have beds for patients to stay overnight.
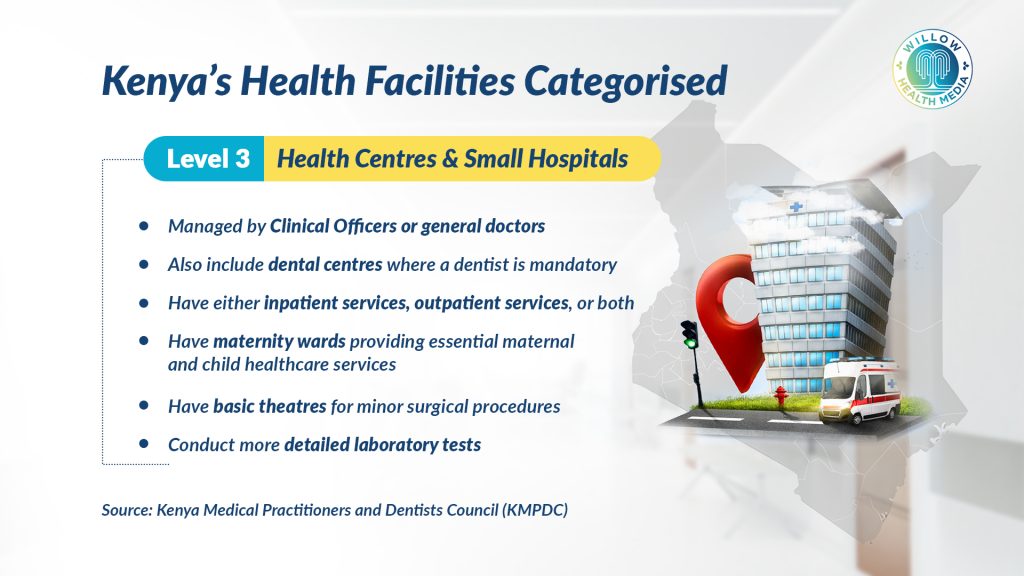
At Level 3 facilities, basically Health Centres and Small Hospitals, the highest level of training is often a clinical officer – a healthcare worker trained to diagnose and treat common conditions, or sometimes a general doctor.
Level 3 facilities “can provide outpatient services only, or even maternity,” Dr Kariuki clarifies, and they are “the first to generally offer inpatient services, often including maternity wards and basic theatres for minor procedures” requiring more attention than a dispensary can provide, including basic lab tests, making them crucial local hubs for essential care.

Level 4 has Sub-County Hospitals or Primary Care Hospitals staffed with medical doctors who are general doctors, besides “specialists like gynaecologists, paediatricians, or surgeons, based on human resources,” notes Dr Kariuki.
These hospitals are the primary referral points within their sub-county, capable of admitting patients for a broader range of medical illnesses beyond maternity, like uncontrolled diabetes or broken limbs, and offering services like X-rays and broader surgical units.

Level 5 facilities are the major County Referral Hospitals, often offering highly specialised care, with the leadership comprising medical professionals, often Chief Executive Officers (CEOs), overseeing extensive inpatient capacities (frequently over 100 beds).
There’s a wide array of specialists, including “sub-specialists like gynaecologists who have training in women’s cancers, or a surgeon trained in orthopaedics, but then you will find some of these in Level 5 or 6,” Dr Kariuki explains.
They provide advanced diagnostics (detailed tests to identify diseases), major surgeries, intensive care for critically ill patients, and specialised consultations.
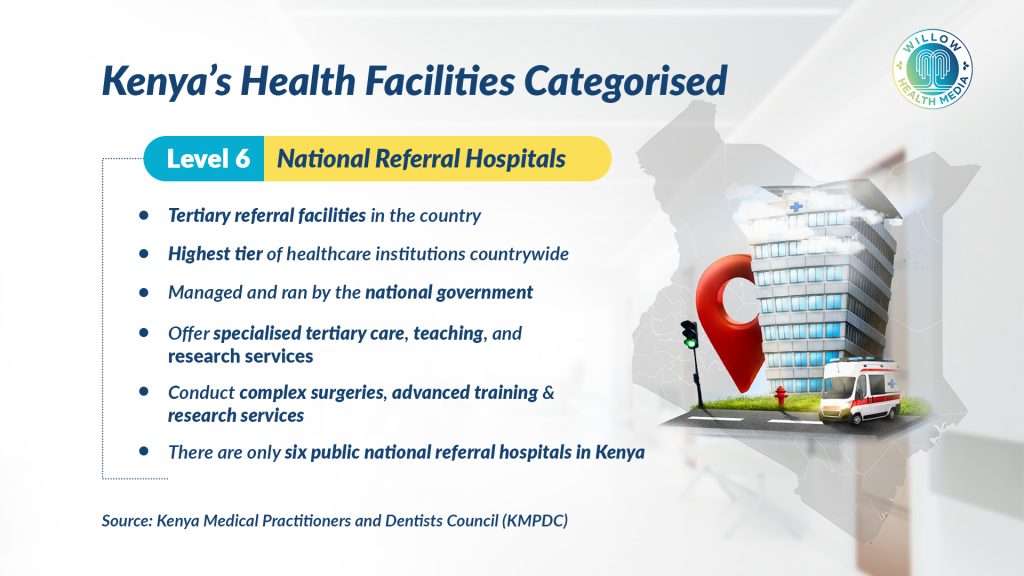
Level 6 are National Referral Hospitals at the very top of the healthcare system. They are managed by the national government.
“If it is a professor of surgery, being the highest skill in the country, will most likely be in a Level 6 such as Kenyatta National Hospital or Nairobi Hospital, the Aga Khan or the Mater Hospital, among others that are providing tertiary services including training other doctors,” Dr Kariuki explains.
These facilities house super-specialists, for instance, an orthopaedic surgeon specialising only in hand bones, and are pivotal centres for advanced treatments, national training and medical research. Top specialists, complex surgeries, advanced training. Examples: KNH, MTRH, Aga Khan, Mater.
Infrastructure is a key factor in determining the level of the facility
Human resources are not enough, as Dr Kariuki states that those people have to work in a certain environment and therefore, infrastructure becomes a key factor in determining the level of the facility.
“A Level 2 might have just two rooms, while a Level 3 could feature more nurses, a small laboratory, and even a small theatre for deliveries.”
He, however, clarifies that when the required rooms are not available, there is an allowance for improvisation such that a particular service can be offered in a room allocated for another service, but there should be discretion and privacy for the patients.
“For example, if a facility decides to offer family planning services in the same room as the post-maternity care, there should be a screen separating where these services are being offered, such that patients get their privacy while getting these services, as the facility finds a separate room,” he adds.
A Level 4 facility admits patients for a wider range of conditions and bed capacity, when matched with appropriate staffing, also indicates a higher level.
Crucially, he states, inpatient facilities across all levels must ensure a 24-hour oxygen supply, either through a cylinder or a dedicated plant, so no patient should lack.
Additional services such as sophisticated laboratories with resident pathologists (doctors who study diseases in laboratory samples) at Levels 5 and 6, and reliable ambulance services further show a facility’s capabilities.
Rigorous oversight means facilities can be downgraded if services decline, or upgraded based on significant new investments
To ensure consistent quality, the KMPDC conducts compliance inspections every one or two years, covering public, private and faith-based facilities.
“How the facility was at the beginning is the promise that you want to provide to the population, so we have to come to check whether you are still keeping that promise for better or worse,” Dr Kariuki emphasises.
This rigorous oversight means facilities can be downgraded if services decline, even if infrastructure remains, or upgraded based on significant new investments in human resources, equipment, and services.
While resources may sometimes limit widespread inspections, the KMPDC actively encourages self-reporting, fostering a culture of accountability within Kenya’s dynamic healthcare landscape. This system ensures that patients receive care at the right level while preventing overcrowding at higher-level facilities with cases that can be handled at lower levels.






















