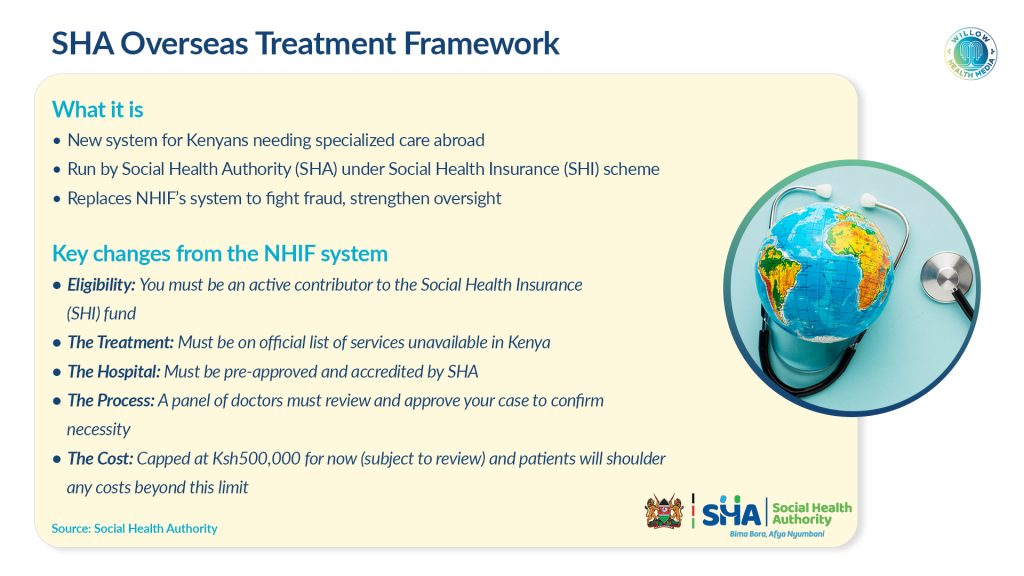
There are 36 listed medical services, and eligible patients must have updated Social Health Insurance payments and use SHA-approved facilities overseas.
The Kenyan government has launched a new framework for overseas medical treatment, capping funding at Ksh500,000 per patient while officially listing 36 medical services unavailable in the country.
Health Cabinet Secretary Aden Duale announced the initiative through the Social Health Authority (SHA), stating it ensures “no Kenyan is denied access to life-saving medical and surgical procedures that are not available locally.”
Duale added that the new framework is the culmination of a rigorous, systematic, and evidence-based assessment by the Benefits Package and Tariffs Advisory Panel (BPTAP), which identified four main categories of locally unavailable treatments, including Joint and Bone Surgery, including wrist, hand and ankle joint replacements, major bone replacements and bone grafts.
The other category is Transplants and Major Surgery, including Liver and bone marrow transplants, children’s kidney transplants, complex heart surgery requiring life support machines, and voice box transplants. The third category is Advanced Cancer Treatment, encompassing specialised radiation therapy, immune cell treatments and advanced diagnostic scans.
Finally, there is Unborn Baby Procedures comprising various intrauterine procedures like blood transfusions, fluid removal and complex surgical interventions.
This preliminary list, which is subject to continuous review and will be guided by a comprehensive health technology assessment (HTA), serves as the official benchmark for approving overseas treatment.
The programme, which takes effect immediately, represents a complete overhaul of Kenya’s overseas treatment system following widespread fraud under the previous National Health Insurance Fund (NHIF).
To qualify for overseas treatment, patients must:
- Have up-to-date Social Health Insurance contributions
- Require treatment for one of the 36 listed unavailable services
- Use SHA-contracted facilities abroad
- Receive treatment that falls within the Ksh500,000 limit
The Claims Management Office will vet all referrals “to ensure medical necessity,” while overseas facilities must be accredited in their home countries and linked to Kenyan hospitals for follow-up care.
The new system directly addresses corruption that plagued the NHIF. Parliamentary investigations revealed NHIF lost about Ksh 21 billion through fraud, with an additional Ksh368 million lost through overpayments blamed on “typing errors” shortly before SHA’s launch.
A parliamentary report found “NHIF could have lost up to Ksh1.7 billion in exaggerated claims and ineligible claims, out of Ksh5.78 billion worth of requisitions.”
The previous system was characterised by lack of oversight, with allegations that a single NHIF staff member approved over 60 per cent of overseas pre-authorisations and was allegedly sponsored on multiple trips to India by some hospitals.
Unlike the previous system, the SHA framework includes:
- A legally mandated, gazetted list of unavailable services
- Peer review mechanisms for all referrals
- Mandatory contracts with overseas providers
- Continuous health technology assessment for updating the list
- Requirements for overseas facilities to link with Kenyan hospitals
The Social Health Insurance Act 2023 provides the legal foundation, requiring SHA to only pay officially empanelled providers with contracts.
While the new framework aims to prevent fraud, it may create delays for critically ill patients. The pre-authorisation process, though designed to ensure medical necessity, could prove lengthy and complex for patients requiring urgent care.
The explicit acknowledgement of these 36 unavailable services also highlights significant gaps in Kenya’s healthcare infrastructure, leaving vulnerable patients dependent on a potentially bureaucratic system to access life-saving treatment abroad.
The Ksh500,000 cap, whilst preventing excessive costs, may prove insufficient for some complex procedures, though the ministry indicates this limit is subject to review following rate negotiations with accredited providers.





















