If the Bill becomes law, drug users will be entitled to subsidised harm reduction services, including rehabilitation, medically assisted therapy, and free commodities such as sterile needles and syringes
People with substance use disorders and those struggling with addiction could soon get access to free medically assisted therapy, counselling and rehabilitation services, if the Harm Reduction Bill 2025 becomes law.
The Bill, tabled in Parliament by Nairobi Woman Representative Esther Passaris, aims to integrate essential healthcare interventions for people with substance disorders into Kenya’s healthcare system.
“A person with substance abuse disorder shall be entitled to harm reduction services such as commodity distribution in the needle and syringe program; medically assisted therapy, HIV-related healthcare services and sexually transmitted infections treatment and prevention services,” the Bill proposes.
It further proposes a shift from punitive measures to a human rights and health-based approach in line with Article 43 of the Constitution of Kenya, meaning that people found guilty of abusing drugs and substances will be treated as patients rather than criminals. This, it states, will reduce any form of discrimination and victimisation.
The Bill is aimed at introducing into the country’s legislative system public health policies and strategies that will reduce negative social or physical consequences of drug use by providing a safe space for persons with substance use disorders.
Passaris’ Bill also proposes health interventions to assist users of drugs and substances in preventing the transmission of infectious diseases like HIV and Hepatitis C through the sharing of needles used to administer intravenous drugs.
The Bill will oblige the Cabinet Secretary of Health to establish harm reduction facilities adequately staffed with trained healthcare providers and equipment. Healthcare providers to be deployed in these facilities will be trained in the treatment, after-care, rehabilitation and social reintegration of persons with substance use disorders.
Public hospitals will be required to maintain a register indicating the number of persons with substance use disorders
Other benefits for persons with substance use disorder include counselling services and the provision of crisis management support. Care providers may refer to the registry for verification of membership of individuals in harm reduction services.
Besides the national government’s legal framework, the Bill proposes that county governments integrate harm reduction services for persons with substance use disorders into their health system.
The draft legislation recognises that county governments are responsible for devolved health functions as stipulated by the Constitution. It highlights other core functions of the national and county governments and areas of collaboration in ensuring the harm reduction services are offered to every Kenyan in need of them.
“The Cabinet Secretary (Health) will develop a comprehensive policy and a national strategy on harm reduction and ensure improved general welfare and treatment of persons with substance disorder,” reads the Bill.
It also stipulates that, within six months of the Act coming into force, the health CS will develop a policy and strategy on the delivery of harm reduction services in public hospitals and maintain a register indicating the number of persons with substance use disorders.
The register will capture the age, sex, disorders or diseases diagnosed and the number of deaths of persons with substance use disorder.
If assented, the law will compel the national government to develop harm reduction standards, provide necessary resources for harm reduction services at national referral facilities and facilitate research and analysis, which are crucial for informing suitable interventions.
“The Cabinet Secretary will designate a directorate under the Ministry of Health to coordinate the provision of harm reduction services in the country,” reads the Bill.
The counties, on the other hand, will be required, through the County Executive Committee (CEC) member in charge of health, to implement the national policies and standards of harm reduction services.
“The CEC will be required to facilitate the provision of harm reduction services within county health facilities, mobilise and allocate resources and funds for delivery of harm reduction services,” the Bill adds.
With the assent of the Act, counties will be responsible for creating awareness of the consequences of substance consumption.
The average initiation age for tobacco, alcohol, khat (miraa), cannabis, cocaine, heroin and prescription drug use in Kenya is between 16-20 years
The Bill comes at the back of grim statistics of substance use in Kenya published in the 2022 report by the National Authority for the Campaign Against Alcohol and Drug Abuse (NACADA), which showed that the initiation age to heroin was 18 years and cocaine 20 years.
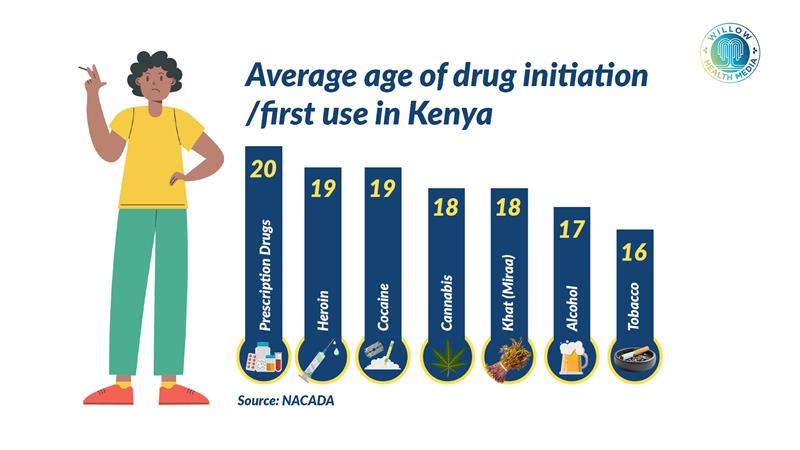
The report titled National Survey on the Status of Drugs and Substance Use in Kenya Abridged Version further states that the average initiation age for tobacco, alcohol, khat (miraa), cannabis, cocaine, heroin and prescription drug use was between 16 and 20 years.
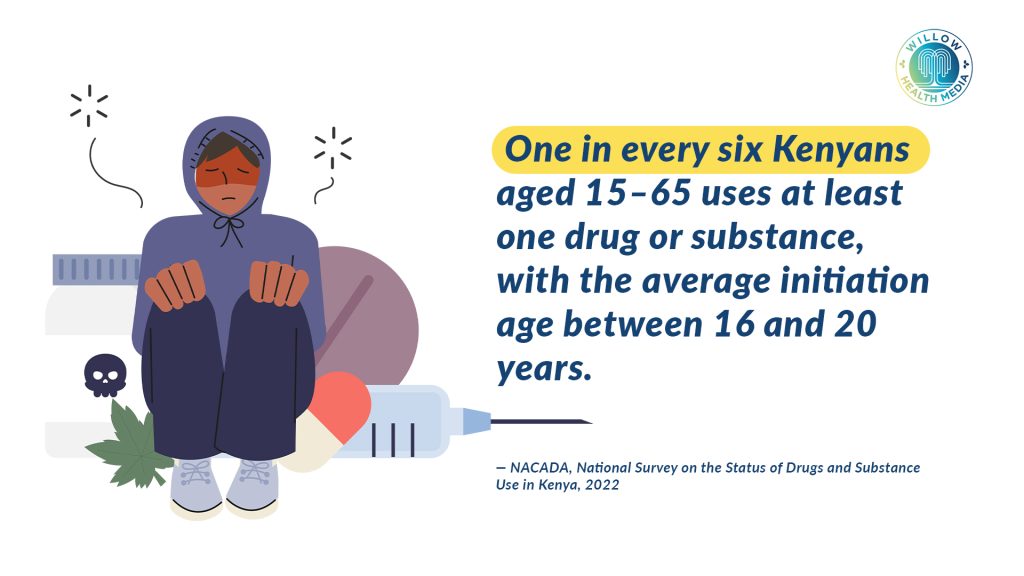
According to the report, one in every six Kenyans aged between 15 and 65 was using at least one drug. One in every three males aged 15-65 years and one in every 16 females were using at least one drug.
The survey found that the western Kenya region had the highest prevalence of the use of at least one drug or substance of abuse (26.4 per cent), followed by Eastern (20.7 per cent) and Nairobi (19.1 per cent).
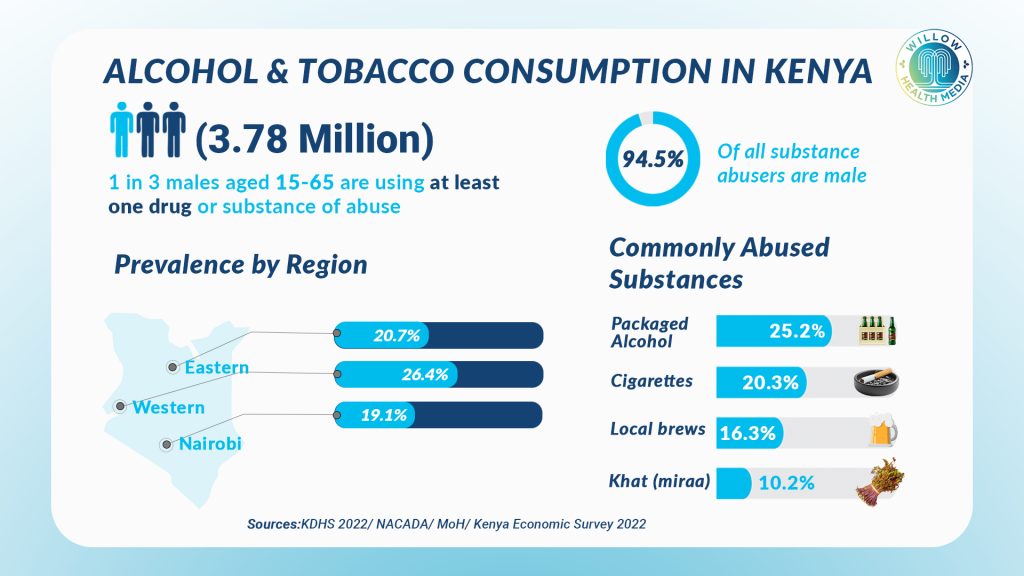
It also established that one in every 8 Kenyans aged 15-65 years was using alcohol. Overall, western Kenya had the highest prevalence of alcohol (23.8 per cent), followed by Coast (13.9 per cent) and Central Kenya (12.8 per cent).
Kenya’s approach to substance use management has elicited intense debate in the past, and this Bill contrasts some aspects of the Cabinet’s National Policy on Prevention of Alcohol, Drugs and Substance Use 2025.
While the National Policy on Prevention of Alcohol, Drugs and Substance Use 2025 allows for the adoption of harm reduction “as applicable”, it has been criticised by civil society for being conservative and failing to make a concrete, explicit commitment to establishing stand-alone interventions like Needle and Syringe Programmes (NSP) or Opioid Substitution Therapy (OST) as community-wide programmes.
Advocacy groups, including the Women Who Use Drugs and Recovering Addicts Development Association (WRADA) and VOCAL Kenya, have been persistently urging lawmakers to adopt a national harm reduction bill, arguing that without explicit commitments in law, vulnerable communities would be bypassed.
According to the United Nations Office on Drugs and Crime, empirical evidence from an Amsterdam cohort showed that Needle and Syringe Programmes plus Opioid Substitution Therapy reduced HIV incidence by 57 per cent and Hepatitis C incidence by 64 per cent.
Needle and Syringe Programmes (NSP) provide sterile needles, syringes, and other injecting supplies such as filters or alcohol swabs either free or at very low cost. They also offer safe disposal of used equipment to prevent reuse and are often integrated with education on safer injecting practices and referrals to treatment, testing, and social services.
Studies show up to 80 per cent reductions in HIV incidence among people who inject drugs when NSP coverage is high.
Like NSP, Opioid Substitution Therapy helps to stabilise people with opioid dependence by replacing illicit opioids like heroin. with a medically supervised, longer-acting opioid such as methadone or buprenorphine. The replacement opioid is taken under medical supervision, helping to prevent withdrawal and cravings without the rapid highs and lows of street opioids.
OPS has been associated with reduced mortality, crime, and overdose and improved social reintegration, while also reducing mortality by 50-70 per cent.
Passaris noted that the Bill, which will not put additional strain on public funds, will reduce negative social or physical consequences of drug use, incorporating a spectrum of strategies including safer use, managed use and abstinence.























