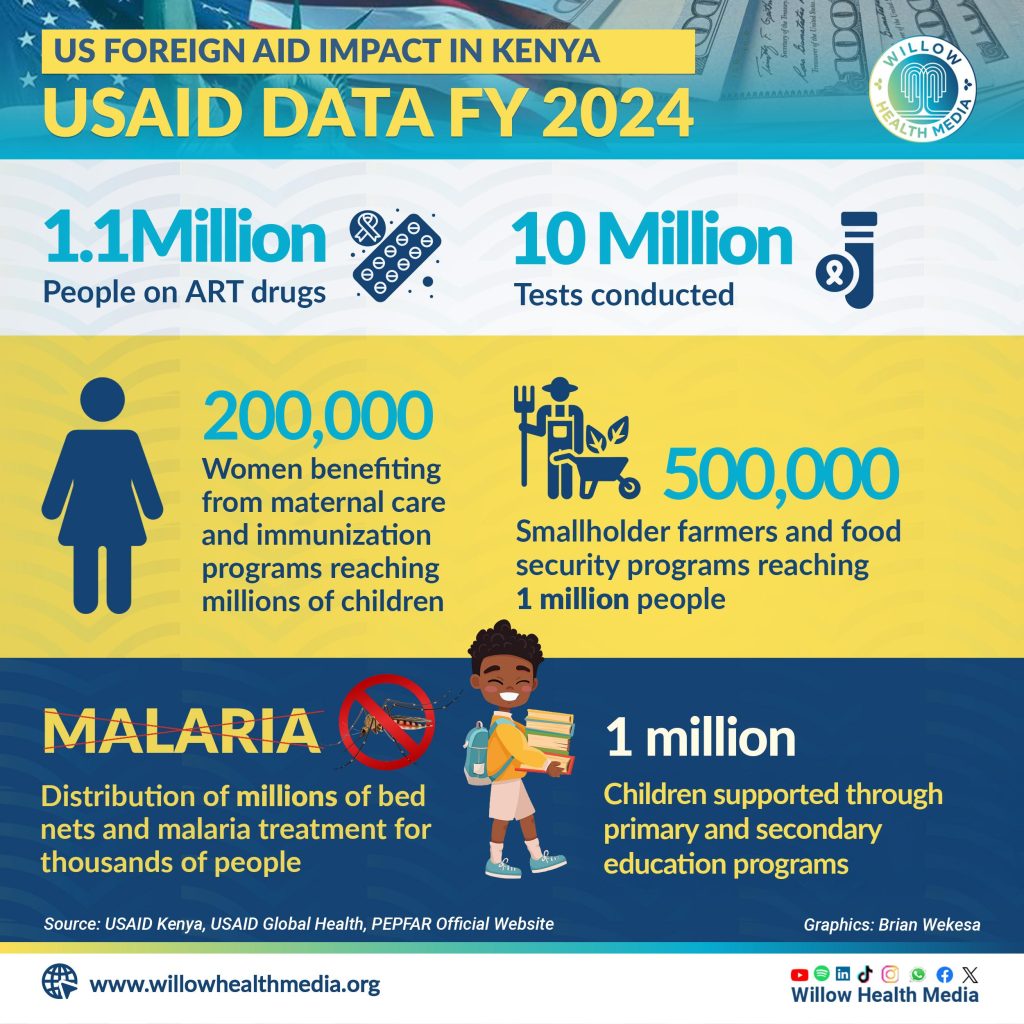
Before Trump’s Order, USAID had procured 320,000 doses of malaria treatment for distribution in Kenya, 4.9 million Long Lasting Insecticidal Nets and five million rapid diagnostic tests
Eric Okioma has lived with HIV for 22 years, since 2003 when he was first diagnosed. For him, it has been a long journey of fear, hope, and the struggle – literally – to stay alive.
Today, getting access to life-saving Antiretroviral (ARV) therapy and treatment is easier since the drugs and commodities are available free of charge in public healthcare facilities and other access points. But back then, it was an uphill task.
“Back then, I had to buy my ARVs out-of-pocket including paying for liver and kidney function tests. This was a huge burden in a country where many live below a dollar a day.”
At the time, ARVs were not available in public facilities and only those participating in clinical trials had access.
Okioma says “I used to spend Ksh6,000 a month for ARVs, Ksh4,000 for liver tests, Ksh4,000 for kidney tests, and Ksh6,000 for CD4 count tests, all on a monthly basis. Unless you had Ksh30,000 – Ksh40,000, you were out of luck.”
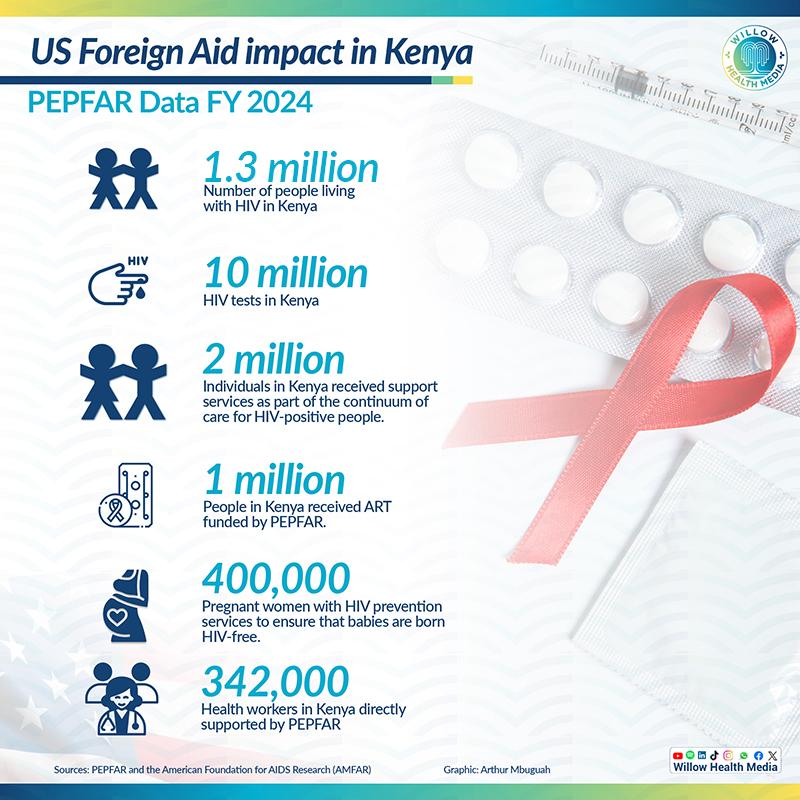
Okioma, who is currently the Team Lead of the Nelson Mandela TB/HIV Information Community Based Organization (CBO) in Nyalenda, Kisumu County, is among more than 1.3 million Kenyans currently living with HIV, and who benefit directly from donor programmes funded heavily by the United States (US) government.
According to data from Aid Data Network, the US government aid to Kenya is approximately U$1.68 billion dollars (Ksh252 billion) annually, out of which U$1 billion dollars (Ksh129.4 billion) is direct aid.
US-funded health programmes from the US Agency for International Development (USAID), Centres for Disease Control and Prevention (CDC) and President’s Emergency Plan For Aids Relief (PEPFAR), the world’s leading HIV initiative, support millions of Kenyans, including those receiving treatment for tuberculosis (TB) and malaria.
This funding covers essential services like Pre-exposure prophylaxis (PrEP) drugs, counselling, testing, and Antiretroviral therapy and treatment.
These organisations felt the shockwaves from US President Donald Trump’s freeze on foreign aid. And while the US Secretary of State’s decision to approve an ‘Emergency Humanitarian Waiver’ has provided a lifeline to the Kenyans living with HIV to continue accessing life-saving HIV treatment, Okioma argues that HIV is complicated by opportunistic diseases and the unfolding health crisis is far from over.
For instance, the Nelson Mandela TB/HIV Information CBO, which was established in 2014, focuses on assisting individuals living with HIV and TB. “About 70-80 per cent of our programmes depend on support from USAID,” explains Okioma, adding that a disruption in funding could mean “more deaths among people with HIV and increase in infections to alarming levels.”

Dr Patrick Amoth, the Director General of Health, had earlier claimed that HIV drugs in Kenya would last for six months, which Okioma disputes from frequent stockouts and calls for increased domestic funding for health programmes.
He also wants parliamentarians to propose a motion banning the dependence of HIV programmes on donor funding for HIV management and treatment.
Trump’s order could have affected HIV programmes in Kisumu County, which has the second-highest prevalence of HIV in Kenya at 14 per cent, according to Dr Gregory Ganda, the Kisumu County Executive Committee Member (CECM) for Medical Services, Public Health, and Sanitation.
That translates to 115,000 people living with HIV who are under treatment and management of HIV in 153 health facilities, with over 1,000 medics who depend on the programme for their salaries spread across public, private and mission hospitals.

Dr Ganda says Trump’s Stop-Work-Order could have caused a major disruption to a planned takeover of some services provided by USAID, including “Human Resources and putting up of a viral laboratory at Kisumu County Referral hospital.”
The planned transition had been underway for two years and included “hiring 1,048 health care workers in which the county has 448 medics, the rest are in mission and private hospitals,” says Dr Ganda, adding that the annual salary of the 448 county healthcare workers totalled Ksh204 million from the USAID HIV programme.
Dr Ganda said the programmes also target preventive measures, especially for the 6,000 commercial sex workers registered by the county who receive condoms, PrEP and advice, and who get services from nine healthcare facilities set aside for special populations, which would have been closed.
Dr Ganda says had the Stop-Work-Order been effected, the programme would have had only salaries for one month without enough time for an alternative business plan. Yet, the Kisumu County human resources is “already high, gobbling up to 40 per cent of the county budget, way above the recommended 35 per cent.”
The order could have financially strained Mission hospitals which care for about 15,000 HIV patients, besides disrupting transportation of viral load samples supported by the US for which the county had set aside Ksh10 million thus crippling the provision of essential services.
Also affected are malaria programmes, with malaria still being a leading killer disease in the country, with at least 70 per cent of the population at risk of contracting malaria, according to the Ministry of Health.
The Global Fund Results Report 2024, published in September and released on December 19, last year shows that deaths associated with malaria increased by 20 per cent as compared to the previous years, from 10,000 in 2010 to 12,000 in 2022.
However, the US Presidential Malaria Initiative report by USAID indicates that Kenya had made significant strides in reducing the malaria burden between 2010- 2020, in which the prevalence had reduced by 50 per cent from 38.1 per cent-18.9 per cent in the lake region area, that has the highest burden of malaria. Nationally, the malaria burden had decreased from 49 per cent to 5.8 per cent.
Before Trump’s Order, USAID had already procured 320,000 doses of malaria treatment for distribution to health facilities in the country, 4.9 million long-lasting insecticide-treated Nets, and five million rapid diagnostic tests, and also protected over 1.5 million people from malaria infections through indoor residual spraying.
The waiver though, revokes President Donald Trump’s Stop-Work-Order for 90 days on January 20, which could have seen a freeze on all USAID, is the other major financier and mainly focuses on reduction of new HIV infections, testing, management and treatment of HIV.
Trump’s freeze on health financing also included the withdrawal of US membership and funding of the World Health Organization (WHO).