Gospel musician Betty Bayo and former MP for Makadara Dick Wathika succumbed to leukaemia, and Dr Elizabeth Kagotho, a hematopathologist, says, “We need to increase awareness, so people recognise symptoms early and know where to seek care” besides investing in diagnostic labs and access to treatment.
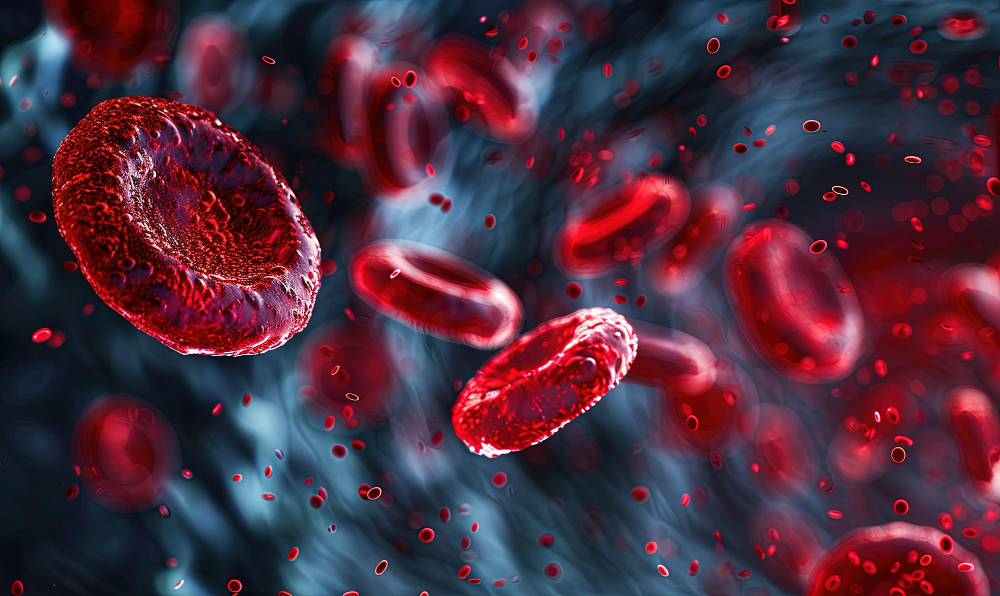
Leukaemia is a type of blood and bone marrow cancer, known as “liquid cancer” because it spreads through the bloodstream instead of forming a solid tumour. Its impact in Kenya is tragically illustrated by its public figures, including gospel musician Betty Bayo and former Member of Parliament for Makadara Dick Wathika, who both succumbed to the disease.
Despite being a growing health concern, public awareness about leukaemia remains very low, leading many patients to seek medical help only when their symptoms are already advanced.
Dr Elizabeth Kagotho, assistant professor and consultant hematopathologist at Aga Khan University Hospital, Nairobi, explains: “The bone marrow is where all our blood cells are produced: white blood cells to fight infections, red blood cells to carry oxygen, and platelets to help the blood clot. When leukaemia develops, abnormal cells called blasts multiply uncontrollably and fail to mature, crowding out normal cells and disrupting the body’s balance.”
The abnormal cells in leukaemia crowd out the bone marrow, suppressing the production of healthy blood cells. This leads to three primary problems: a lack of red blood cells causes persistent fatigue, a deficiency in white blood cells results in frequent infections, and a shortage of platelets increases the risk of bleeding and easy bruising.
Leukaemia is categorised by how fast it spreads and by type of white blood cell affected
“Patients often complain about being unable to do the work they used to do, or experiencing repeated infections,” says Dr Kagotho.
“Some may notice blood when brushing their teeth or small red spots under the skin. Bone pain or swollen lymph nodes can also occur, and sometimes patients experience unexplained weight loss or night sweats.”
Leukaemia is categorised in two main ways: by how fast it progresses and by the type of white blood cell affected. These types are described below.
Classified by speed
- Acute: Progresses rapidly with immature cells; requires aggressive, immediate treatment.
- Chronic: Develops slowly; symptoms appear gradually over time.
Classified by cell type
Leukaemias are further divided based on whether they affect myeloid cells (which include neutrophils) or lymphoid cells (like B and T lymphocytes).
- Acute Myeloid Leukaemia (AML): Rapid cancer of myeloid cells; more common in Kenyan adults.
- Acute Lymphoblastic Leukaemia (ALL): Rapid cancer of lymphoid cells; most common in Kenyan children, usually the B-cell type.
- Chronic Myeloid Leukaemia (CML): Slow-progressing cancer of myeloid cells; more common in adults.
- Chronic Lymphocytic Leukaemia (CLL): Slow-progressing cancer of lymphoid cells; more common in adults.
“The exact causes of most leukaemias are unknown,” Dr Kagotho notes. “However, mutations in the DNA of bone marrow cells play a central role. Think of DNA as the cell’s instruction manual. When it is damaged, cells may grow uncontrollably, fail to mature, and avoid programmed cell death.”
While most leukaemias are not directly linked to lifestyle, some risk factors are recognised:
- Age: Risk increases, particularly for acute leukaemias, in people over 60.
- Radiation exposure: High-dose radiation increases leukaemia risk.
- Chemical exposure: Occupational exposure to substances like benzene is linked to leukaemia.
- Prior cancer treatment: Chemotherapy or radiotherapy can predispose patients to secondary leukaemia.
- Genetic predisposition: Certain syndromes, such as Down syndrome, increase the likelihood of leukaemia.
- Smoking: Cigarette smoking is associated with acute myeloid leukaemia due to carcinogens.
Symptoms of leukaemia are often vague, mimicking common illnesses, which can delay diagnosis. But here are common Symptoms:
- General: Persistent fatigue, unexplained weight loss, and night sweats.
- Infection & Bleeding: Frequent infections, unexplained bleeding, and small red spots under the skin.
- Pain & Swelling: Bone pain and swollen lymph nodes.
Key Diagnostic Steps
- Initial Test: A Complete Blood Count (CBC) checks levels of red cells, white cells, and platelets.
- Visual Check: A Blood Smear under a microscope looks for abnormal immature cells (blasts).
- Confirmation Test: A Bone Marrow Aspirate or Biopsy confirms the presence and type of leukaemia.
- Specialised Analysis: Flow cytometry and genetic tests classify the exact subtype and guide treatment.
“Mutations in leukaemia cells are highly variable,” explains Dr Kagotho. “Some indicate a favourable prognosis, while others suggest a higher risk and may require stem cell transplantation. Personalised testing is crucial to guide treatment.”
Chemotherapy remains the cornerstone of leukaemia treatment. Acute leukaemias require intensive, multi-phase chemotherapy to eradicate rapidly growing blast cells. Targeted therapies, such as imatinib for chronic myeloid leukaemia, are available in Kenya and have dramatically improved outcomes, allowing patients to live near-normal lives.
Bone marrow transplantation, though available in select private hospitals, remains costly and sometimes inaccessible to many patients. Insurance coverage, both private and national, plays a critical role in accessing treatment.
“While chemotherapy and targeted therapy are generally accessible in major public referral hospitals like Kenyatta, Moi Teaching, and Aga Khan University Hospitals, the cost and availability of bone marrow transplantation remain a barrier for most patients,” Dr Kagotho notes.
Survival for leukaemia patients varies significantly by type and is affected by delayed diagnosis and healthcare access in Kenya.
- Chronic Myeloid Leukaemia (CML): Patients on targeted therapy can have a near-normal life expectancy.
- Acute Lymphoblastic Leukaemia (ALL) in Children:
- Global Survival: 80–90%
- Outcome in Kenya: Significantly lower due to late diagnosis, limited supportive care, and financial barriers.
- Acute Myeloid Leukaemia (AML):
- Global Survival: Approximately 60%
- Outcome in Kenya: Also lower for the same reasons.
Available data indicate a significant annual leukaemia burden, but the true number is likely higher.
Based on Kenya’s 2024 National Cancer Institute data, about 2,000 new cases of acute leukaemia were recorded, making up four per cent of the country’s estimated 47,000 total cancer cases for that year. For a global comparison, the GLOBOCAN 2022 estimate suggests a slightly lower figure of around 1,729 new leukaemia cases, which would represent about 3.9 per cent of all cancer cases nationally.
“Sometimes the data may be underestimated because cases need to be reported to the National Cancer Registry to be officially recorded,” explains Dr Kagotho. “This means the figures might not reflect the full picture. In fact, some patients may tragically succumb to their illness even before a formal diagnosis is made.”
Improving leukaemia outcomes in Kenya requires strengthening health systems
Awareness of leukaemia in Kenya is low. Many patients initially self-medicate or visit local clinics, delaying diagnosis until symptoms are advanced. Dr Kagotho emphasises the need for public education: “We need to increase awareness of leukaemia, so people recognise symptoms early and know where to seek care. Investments in diagnostic laboratories and access to treatment are equally important.”
The path to improving leukaemia outcomes in Kenya requires strengthening its health system by expanding diagnostic capacity and ensuring access to modern therapies. While leukaemia is not the most common cancer, new treatments offer hope. Progress depends on tackling key challenges: raising public awareness for earlier detection and ensuring equitable access to care.
As Dr Kagotho concludes, “This is a call to action: the population needs to understand leukaemia, healthcare systems must provide timely diagnosis and treatment, and investments in specialist laboratories and accessible care are critical. Awareness, early detection, and supportive treatment can dramatically improve survival and quality of life for our patients.”
This explainer was first published by Willow Health Media on December 29, 2025.