Men act as a ‘silent reservoir’ for reinfection, turning a manageable condition into a chronic, soul-crushing cycle of clinical failure.
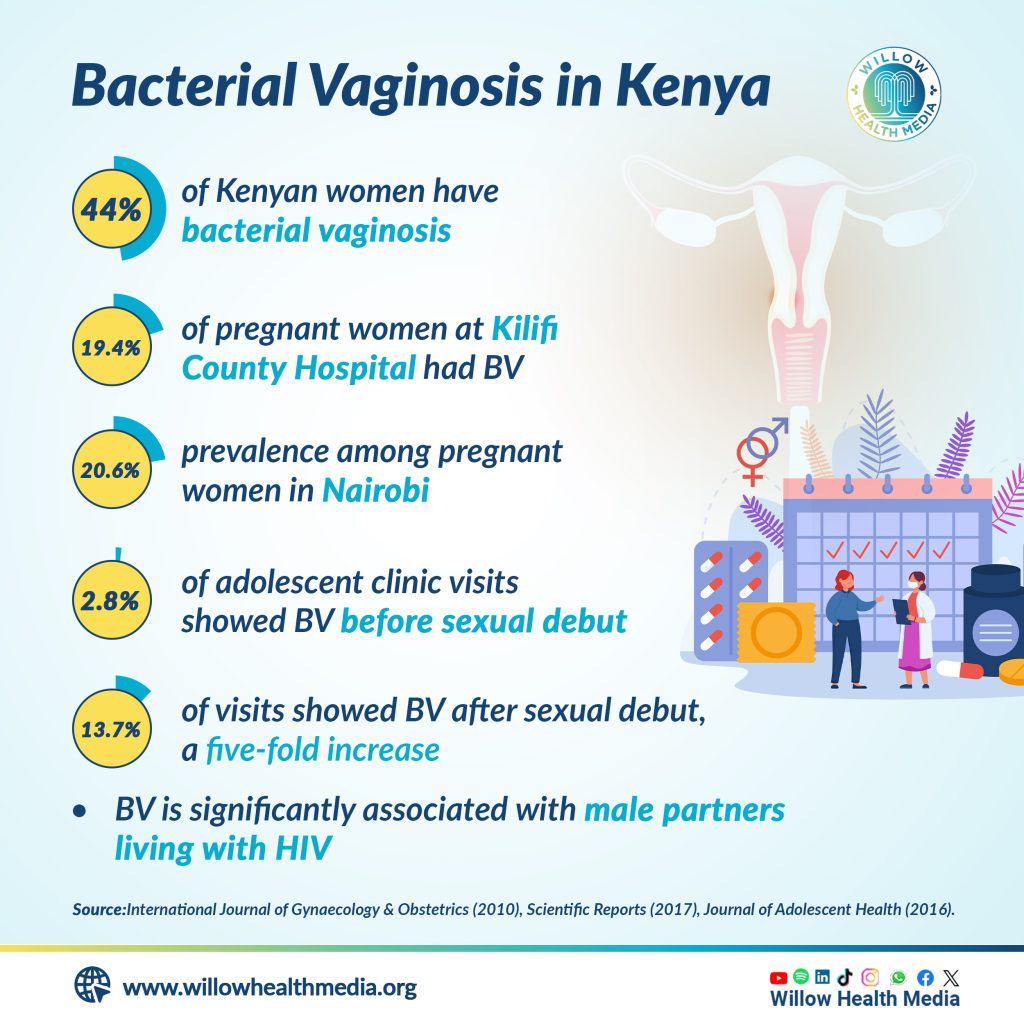
For decades, the medical community viewed Bacterial Vaginosis (BV) through a strictly gendered lens. It was classified as a lonely struggle- a frustrating, “female-only” imbalance of vaginal flora that women were expected to manage in isolation. However, a revolutionary shift in clinical thinking, culminating in landmark research in 2025, is dismantling that narrative.
We now understand that treating a woman for BV while ignoring her male partner is pointless. The latest evidence suggests that in heterosexual relationships, men act as a “silent reservoir” for reinfection, turning a manageable condition into a chronic, soul-crushing cycle of clinical failure.
Consider the case of “Elena,” a 31-year-old educator who spent four years trapped in a cycle of clinical shame. Every few months, Elena would experience the tell-tale symptoms: a thin, grayish-white discharge and a distinct, fish-like odour that flared prominently after intimacy with her long-term partner.
Elena followed every clinical protocol. She took her metronidazole faithfully, switched to pH-neutral cleansers, and wore breathable fabrics. Each time, the symptoms vanished-only to return weeks later. Elena began to feel “biologically broken,” and her relationship suffered as she avoided intimacy to prevent the inevitable return of the infection.
The bacteria causing distress were residing quietly in the urethra, under the foreskin
What Elena and her partner didn’t realize was that he was the missing link. While he had zero symptoms, he was a silent carrier. The bacteria causing Elena’s distress were colonising his anatomy, residing quietly in the urethra and under the foreskin. Every act of intimacy was a “ping-pong” transfer of bacteria that one-sided antibiotics simply could not break.
To understand why men are central to this puzzle, we must look at the vaginal microbiome. A healthy vagina is dominated by Lactobacillus species, which produce hydrogen peroxide and lactic acid to maintain a protective, acidic environment. BV occurs when these protectors are overrun by a complex consortium of anaerobic bacteria, most notably Gardnerella vaginalis.
Gardnerella is particularly insidious because it creates a biofilm, a sticky, protective matrix that allows it to cling to host cells and resist antibiotic penetration. Scientists have now demonstrated that this biofilm is highly transmissible. In heterosexual couples, this biofilm hitches a ride on the male partner, where it survives without causing him any outward irritation, waiting to be reintroduced to the vaginal environment.
The clinical smoking gun arrived with a landmark randomized controlled trial published in The New England Journal of Medicine involving heterosexual couples to test the efficacy of partner treatment:
- The Control Group: Women received standard antibiotics; their male partners received nothing.
- The Treatment Group: Women received standard care, but their male partners received a dual attack: oral metronidazole and two per cent clindamycin gel applied to the glans and upper shaft of the penis twice daily for seven days.
Women are often unaware that their partners are ‘re-seeding’ the infection
The disparity in results was so significant that the trial was halted early for ethical reasons. In the “women-only” group, 63 per cent of participants saw their BV return within three months. In the group where the men were also treated, the recurrence rate plummeted to 35 per cent. This research proved that for millions of women, BV is not a failure of hygiene or personal biology, but a failure to treat the partnership.
Men aren’t being negligent; they are biologically unaware. In the male anatomy, Gardnerella and associated anaerobes rarely trigger an inflammatory response. This creates a dangerous “clinical blind spot.” Because the man feels fine, the woman often bears the entire psychological and physical burden of the condition, unaware that her partner is effectively “re-seeding” the infection.
Severe clinical complications associated with chronic recurrence:
- STI vulnerability: BV disrupts the vaginal lining, significantly increasing the risk of contracting HIV, chlamydia, and gonorrhoea.
- Obstetric risk: For pregnant women, chronic BV is a leading cause of preterm labour and premature rupture of membranes.
- Fertility & IVF: Data suggests BV is associated with tubal factor infertility and lower implantation rates during assisted reproduction.
- HIV Shedding: HIV-positive women with BV have higher viral shedding, increasing the risk of transmission to their partners.
Bacterial Vaginosis is no longer just a ‘vaginosis’ but a relational dynamic
One of the most significant hurdles in treating BV is the formation of the biofilm. Standard oral antibiotics often struggle to penetrate the dense, sticky matrix that Gardnerella constructs on the vaginal wall.
When a woman completes her treatment, the “free-floating” bacteria may be killed, but the biofilm often remains dormant. When she has sex with a partner who is also carrying these bacteria, the new influx acts as a catalyst, “waking up” the dormant biofilm and triggering a full-blown recurrence. By treating the man, we eliminate the external catalyst, giving the woman’s natural Lactobacillus a fighting chance to reclaim the territory.
The American College of Obstetrics and Gynaecology (ACOG) issued a Clinical Practice Update in October 2025. For the first time, it recommends that clinicians consider oral and topical antibacterial treatment for the male sexual partners of patients with recurrent, symptomatic BV.
This change validates the lived experience of millions of women who knew, intuitively, that their infections were linked to their sexual activity, despite being told otherwise for decades.
Bacterial Vaginosis is no longer just a “vaginosis”, it is a relational dynamic. By treating the couple as a single unit, we can move away from ineffective, one-sided protocols and toward a future where both partners are protected.
Request partner treatment: Discuss the benefits of concurrent treatment (oral and topical) for your partner.
Adhere to the full course: Both partners must complete the entire regimen, typically 7 days.
Abstain during treatment: Intimacy should be avoided until both partners have finished their medication.
Focus on restoration: Consider vaginal probiotics containing L. Crispatus to help rebuild the protective barrier.
The shift in how we view BV represents a victory for evidence-based medicine. It acknowledges that the human body does not exist in a vacuum; our health is inextricably linked to those we are closest to.
Dr Madeline Iseren is a pharmacist and commentator on topical medical and health issues.
Graphics by Brian Wekesa.