In addition to preventing illness, emergency vaccine interventions generated an estimated US$32 billion (over Ksh4 trillion) in economic benefits through lives saved and years of productivity gained
Emergency vaccination responses between 2000 and 2023 have led to a 60 per cent drop in deaths from major infectious diseases in low-income countries, a report has revealed.
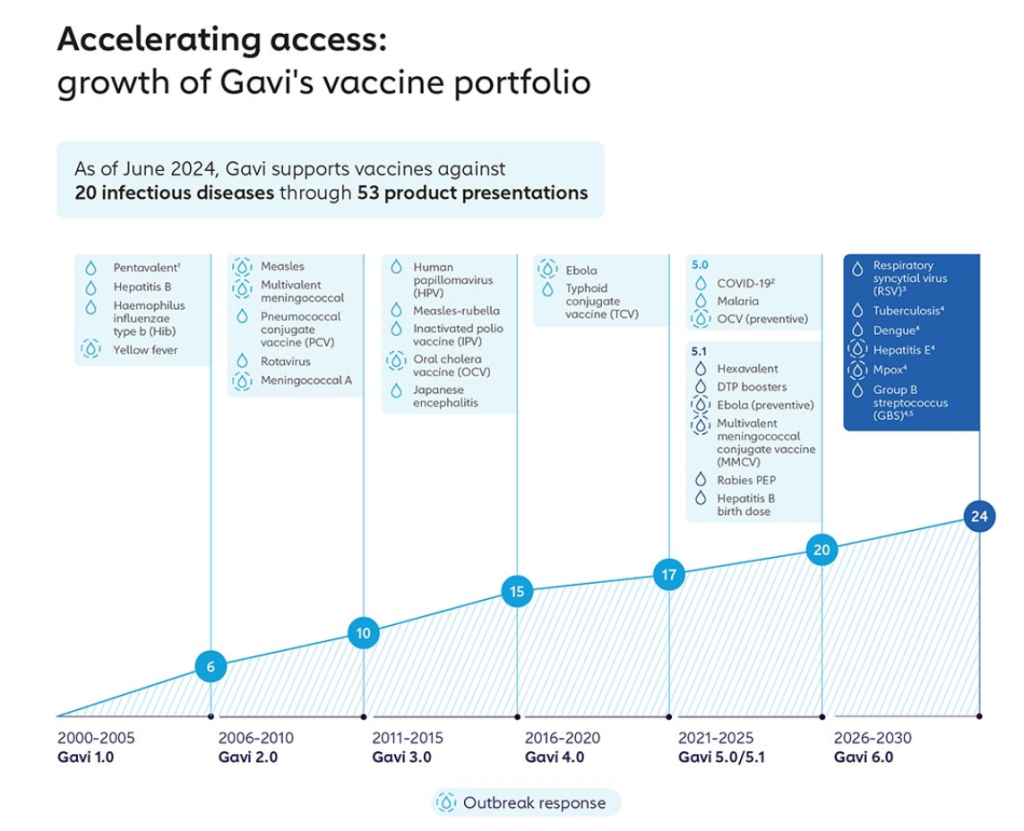
The landmark global study by the Burnet Institute and Gavi, the Vaccine Alliance, details the life-saving and economic impact of emergency vaccination campaigns targeting cholera, Ebola, measles, meningitis, and yellow fever.
The first-of-its-kind research, published in BMJ Global Health, analysed over 210 outbreaks in 49 countries, with results showing that emergency vaccination reduced cases by an average of 57 per cent and deaths by 58 per cent.

In addition to preventing illness, the interventions generated an estimated US$32 billion (over Ksh4 trillion) in economic benefits through lives saved and years of productivity gained.
According to Dr Sania Nishtar, CEO of Gavi, the study comprehensively quantified the benefit, in human and economic terms, of deploying vaccines against outbreaks of some of the deadliest infectious diseases.
“This study demonstrates clearly the power of vaccines as a cost-effective countermeasure to the increasing risk the world faces from outbreaks,” said Dr Nishtar. “It also underscores the importance of fully funding Gavi, so it can continue to protect communities in the next five years to come.”
Rapid vaccine deployment and strong routine immunisation systems prevent outbreaks from escalating
The most significant reductions were seen in yellow fever outbreaks, where cases fell by 98 per cent and deaths by 99 per cent. Ebola emergency vaccinations reduced cases by 77 per cent and deaths by 76 per cent, significantly lowering the likelihood of large-scale epidemics like the 2014 West Africa crisis.
Measles responses yielded 59 per cent fewer cases and 52 per cent fewer deaths, while cholera and meningitis interventions cut cases and deaths by 25–28 per cent on average.
Critically, the study also emphasises the importance of rapid vaccine deployment and strong routine immunisation systems in preventing outbreaks from escalating.
Kenya has been a major beneficiary of Gavi support since 2001, receiving over US$940 million (over Ksh121.4 billion) in vaccines and related supplies. This has enabled the introduction of crucial life-saving vaccines into the national immunisation schedule.
In 2002, Kenya adopted the pentavalent vaccine, contributing to an 89 per cent reduction in Haemophilus influenzae type b (Hib), a major cause of meningitis and pneumonia.
With Gavi’s support, it also became the first African country to introduce the Pneumococcal Conjugate Vaccine (PCV) in 2011, which protects against pneumonia, meningitis and sepsis. Subsequent years saw the addition of the second dose of the measles vaccine, rotavirus, inactivated polio, and malaria vaccines.
Already, Kenya has introduced the Typhoid Conjugate Vaccine (TCV) in an ongoing comprehensive 10-day national vaccination campaign where children aged between nine months and 14 years have been targeted for TCV and the Measles-Rubella (MR) Vaccine.
Community engagement, improved data systems, and targeted outreach cited as key drivers of vaccination coverage
According to UNICEF and WHO data, Kenya’s under-five mortality rate declined from 101 deaths per 1,000 live births in 2000 to 51 in 2015, with vaccines playing a key role.
A 2023 evaluation of Gavi’s Health Systems Strengthening (HSS) support in Kenya found significant improvements in coverage. Between 2017 and 2023, the percentage of sub-counties achieving over 80 per cent Pentavalent Vaccine coverage rose from 30 per cent to 59 per cent.

In 17 historically underserved counties, coverage increased from 27 per cent to 57 per cent. Community engagement, improved data systems, and targeted outreach were cited as key drivers.
Global research shows that every US$1 (Ksh129) spent on vaccines yields up to US$21 (about Ksh2,700) in direct benefits such as reduced treatment costs and up to US$54 (about Ksh6,900) in societal gains, including increased productivity and fewer years lost to illness.
For Kenya, the US$940 million in Gavi support could translate into billions of shillings in cumulative economic returns over time.
Kenya remains at risk of yellow fever outbreaks, particularly in border counties. The global study found that emergency yellow fever vaccination campaigns reduced cases by 98 per cent and deaths by 99 per cent. Maintaining high coverage and quick deployment capacity is crucial, especially in areas where routine immunisation rates are lower.
Despite progress, measles outbreaks continue to affect some regions, especially where routine coverage dips
Kenya has successfully eliminated meningitis A outbreaks through routine immunisation since 2017. However, outbreaks from other meningitis strains remain a threat. The study shows that outbreak response vaccination reduces such cases and deaths by around 27–28%.
Kenya’s adoption of the new multivalent conjugate vaccine effective against five major strains offers a pathway to further controlling and possibly eliminating meningitis outbreaks.
Despite progress, measles outbreaks continue to affect some regions, especially where routine coverage dips. The study confirms that emergency measles vaccination can reduce cases by 59 per cent and deaths by 52 per cent, which are life-saving numbers in informal settlements and remote counties.
Cholera, though not as widespread in Kenya as it is in West Africa, remains a challenge in areas with limited access to clean water and sanitation. The study estimates that cholera emergency vaccinations reduce cases by 28 per cent and deaths by 36 per cent, especially when campaigns are launched quickly.
Although Kenya has not experienced a large-scale Ebola outbreak, the threat remains real due to regional proximity to Uganda and Congo. Modelling data from the study show that swift Ebola vaccination can reduce both cases and deaths by over 75 per cent and drastically limit the spread of large-scale emergencies.
Kenya’s preparedness supported by global vaccine stockpiles and early response financing could prove critical in future scenarios.
Public health experts have called for Kenya to introduce targeted levies and taxes to increase the national immunisation budget
Kenya is entering a critical transition period as it prepares to take full financial responsibility for its immunisation programme by 2030. Currently, Gavi funds around 90 per cent of the programme, while Kenya covers the remaining 10 per cent.
For the 2024/25 fiscal year, the government still owes US$12.49 million (Ksh1.6 billion) in co-financing payments.
Kenya’s immunisation programme currently requires around Ksh11.58 billion (about US$94 million) per year. Of this, Gavi provides Ksh6.5 billion, the US government contributes Ksh585 million, and Kenya’s domestic allocation stands at Ksh2 billion, leaving an annual deficit of about Ksh2.5 billion. Bridging this shortfall will require increased domestic funding and innovative financing strategies.
Public health experts have called for Kenya to introduce targeted levies such as sugar, tobacco, or alcohol taxes and to increase the national immunisation budget from the current 0.5–1 per cent of health spending to at least 3 per cent, in line with global best practices.
Kenya was required to settle its US$12.49 million (Ksh1.6 billion) co-financing obligation by June this year to avoid vaccine stockouts and enhance outbreak readiness, but this payment remains pending.
As Gavi support phases out by 2030, Kenya now needs sustainable domestic financing from sources such as increased health budget allocations and innovative taxes on sugar, tobacco or alcohol to replace donor contributions.
Maintaining high routine immunisation coverage and rapid emergency response capacity is critical to preventing disease resurgence. Continued access to Gavi-funded global vaccine stockpiles and early response funds will also be vital for outbreak control.





















